C Melchior et al. United European Gastroenterology Journal, 2025; 00:1–39. Open Access! European Consensus on Functional Bloating and Abdominal Distension—An ESNM/UEG Recommendations for Clinical Management
A total of 21 experts (authors of article), recommended by ESNM, The European Association for Gastroenterology, Endoscopy and Nutrition (EAGEN) and The European Society for Primary Care Gastroenterology (ESPCG), from different countries agreed to participate as the International Working Group for the European Consensus on Bloating to vote on the Delphi statements.
This article regarding bloating/distension in adults is summarized in two tables. Table 1 has 75 statements. Table 2 is a summary –here are many of its recommendations:
Patients with functional bloating and abdominal distention should receive a lactose‐limiting diet trial based on their self‐reported symptoms or the presence of intolerance during a breath test after ingestion of a defined lactose load
- A low FODMAP diet is effective in reducing functional bloating and abdominal distention
- Rifaximin may be useful for the treatment of functional bloating and abdominal distention with efficacy
- Among antispasmodic agents, pinaverium and otilonium bromide have been shown to be the most effective drugs for the treatment of functional bloating and abdominal distension
- Lubiprostone, plecanatide and linaclotide are effective in improving constipation associated with functional bloating and abdominal distension
- Linaclotide is the most effective secretagogue for functional bloating, although limited data is available for lubiprostone and plecanatide as well
- Selective serotonin reuptake inhibitors (SSRI’s) are effective in reducing symptoms of functional bloating
- Tricyclic antidepressants (TCA) such as amitriptyline are effective in reducing symptoms of functional bloating
- In patients with discrete episodes of visible abdominal distension, biofeedback‐guided techniques to re‐educate abdominothoracic muscular activity are safe and effective for correction of abdominal distention and are associated with improvement in the subjective sensation of abdominal bloating
- “Hypnotherapy improves symptoms of bloating in patients with IBS. However, its effect on functional bloating and abdominal distension was not explored and cannot be recommended”
- Figure 1 provides an algorithm. For workup, it suggests checking the following in all patients: TSH, HgbA1c, CBC, CRP, TTG IgA, IgA, Glucose
- In those with alarm features (eg. anemia, wt loss, suspicion of organic disease), more extensive evaluation is recommended
My take: One of my colleagues would often say that if there are a lot of treatments for a disease it usually indicates that none of them are very good.
Related blog posts:
- Jose Garza: Belching, Bloating and Best Advice
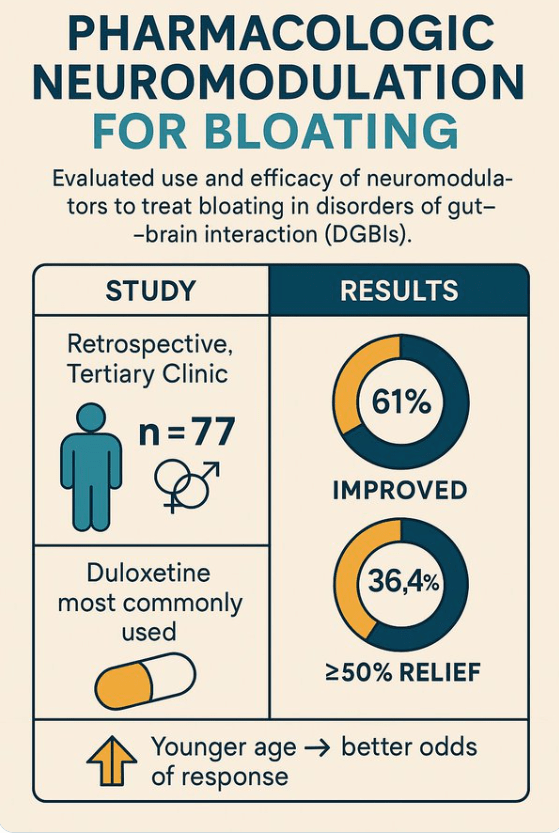
- Pharmacologic Neuromodulation for Bloating Symptoms
- How Common is Bloating?
- Expert Advice on Bloating

Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.