J Orozco et al. Am J Gastroenterol 2025; 120: 1381-1387. Comparison of the Bristol Stool Scale and Modified Version for Children: Use by Providers vs Children
Thanks to Ben Gold for this reference.
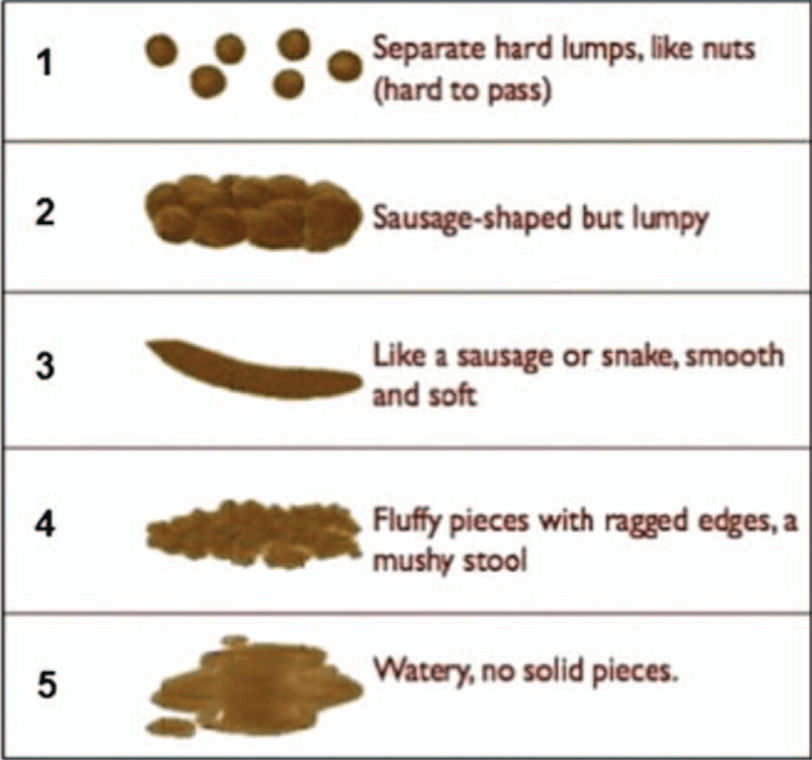
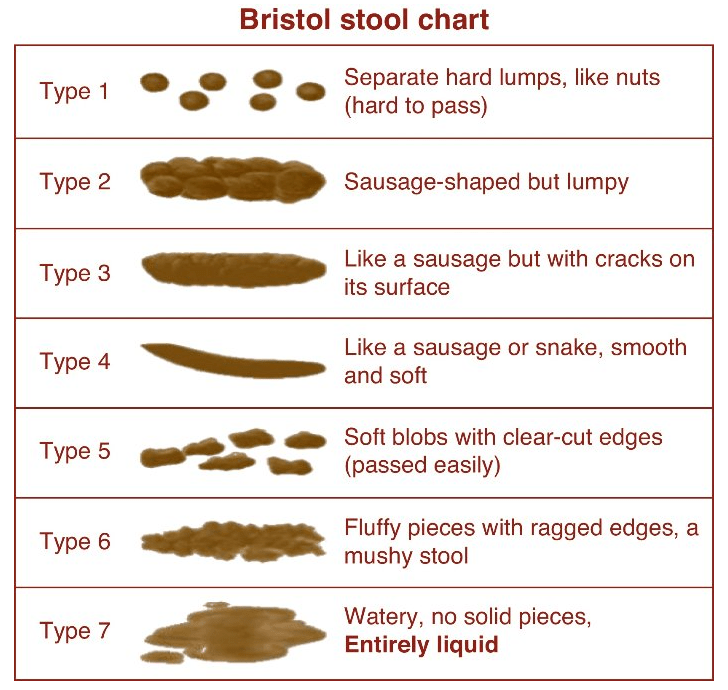
Background: The modified Bristol Stool Form Scale for Children (mBSFS-C) removes #3 and #5 from the Bristol Stool Form Scale (BSFS), leaving only one normal image and shortening the options from seven to five.
Methods: Pediatric gastroenterology providers (21 faculty, 11 fellows, 3 nurse practitioners) and 200 children/families rated the same 35 stool photographs, reflecting diverse stool forms, using both scales. The order of photograph presentation and scale use were randomized.
Key findings:
- Of 1,225 provider ratings using the mBSFS-C, 90.0% agreed with the provider’s modal ratings vs 77.8% using the BSFS.
- Of 7,000 child ratings using the mBSFS-C, 84.6% agreed with the children’s modal ratings vs 71.8% using the BSFS.
- Using providers’ modal ratings as the reference, all mBSFS-C photograph modal ratings matched between children and providers (35/35 photographs) whereas only 86% (30/35 photographs) matched with the BSFS.
Discussion:
- “Unique and new in this study is the direct head-to-head comparison of the 2 scales (BSFS, mBSFS-C) when used by pediatric gastroenterology providers and children. Both the BSFS and mBSFS-C demonstrated excellent reliability…modal rating agreement was significantly poorer for the BSFS than for the mBSFS-C.”
- “Almost 20% of the time expert raters using the BSFS (vs. 8% with the mBSFS-C) deemed a stool to be a different clinical delineation than that selected by the majority of their peers.”
Related editorial: Peter Lu, The American Journal of Gastroenterology 120(6):p 1267, June 2025. Is It Time to Scale Down the Bristol?
My take: The modified BSFS is easier and better. This study indicates it should be widely used for children but probably for adults too. As Dr. Lu’s editorial notes, “aren’t adults just big children?”
Related blog posts: