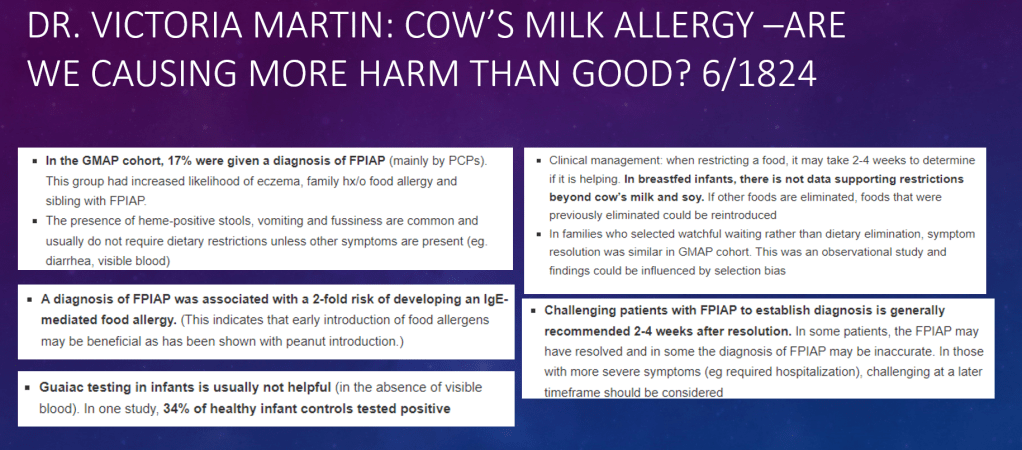
A recent randomized clinical study (M Urashima et al. JAMA Pediatr. 2019;173(12):1137-1145) indicates that avoiding cow’s milk formula in the first 3 days of life may prevent the development of cow’s milk allergy. Thanks to Ben Gold for this reference.
Link to full Abstract (article behind paywall): Primary Prevention of Cow’s Milk Sensitization and Food Allergy by Avoiding Supplementation With Cow’s Milk Formula at Birth
The Atopy Induced by Breastfeeding or Cow’s Milk Formula (ABC) trial, a randomized, nonblinded clinical trial, began enrollment October 1, 2013, and completed follow-up May 31, 2018, at a single university hospital in Japan. The primary outcome was sensitization to cow’s milk (IgE level, ≥0.35 allergen units [UA]/mL) at the infant’s second birthday.
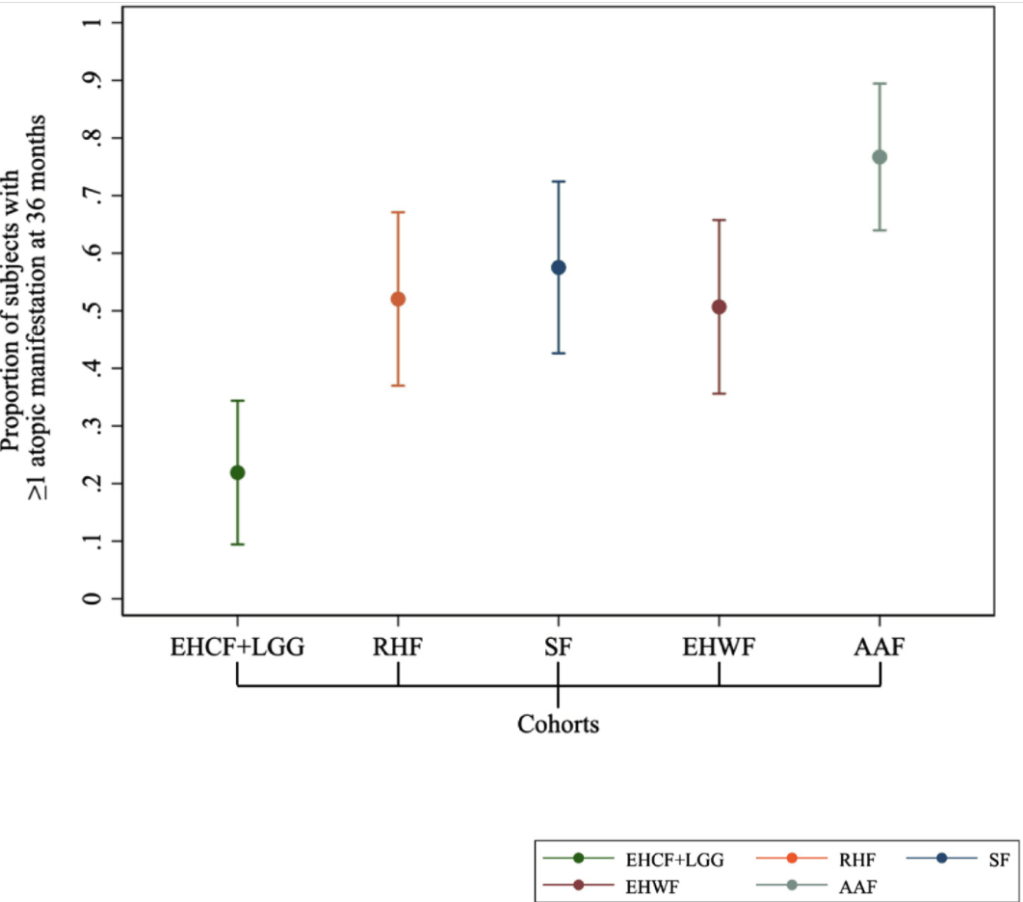
Immediately after birth, newborns were randomized (1:1 ratio) to BF with or without amino acid–based elemental formula (EF) for at least the first 3 days of life (BF/EF group) or BF supplemented with CMF (≥5 mL/d) from the first day of life to 5 months of age (BF plus CMF group).
If the mother, allocated to the BF/EF group, added more than 150 mL/d of EF to BF for 3 consecutive days, EF was switched to CMF after the fourth day. Thus, offspring allocated to BF/EF could avoid CMF for at least the first 3 days of life.
Key Finding:
- “In this randomized clinical trial involving 312 newborns, risks of sensitization to cow’s milk and immediate-type food allergy, including cow’s milk allergy and anaphylaxis, were decreased by avoiding supplementation with cow’s milk formula for at least the first 3 days of life.”
- “The primary outcome occurred in 24 infants (16.8%) in the BF/EF group, which was significantly fewer than the 46 infants (32.2%) in the BF plus CMF group (relative risk [RR], 0.52; 95% CI, 0.34-0.81).”
- “The prevalence of food allergy at the second birthday was significantly lower in the BF/EF than in the BF plus CMF groups for immediate (4 [2.6%] vs 20 [13.2%]; RR, 0.20; 95% CI, 0.07-0.57) and anaphylactic (1 [0.7%] vs 13 [8.6%]; RR, 0.08; 95% CI, 0.01-0.58) types.”
This study is interesting in that it suggests that exposure to cow’s milk in the first three days of life potentially increases the risk of CMA, whereas a previous study (*see below) showed showed that early exposure to CMF within 14 days after birth reduces the risk of CMA. In this previous study, exposure to small quantities of CMF for the first 3 days of life was not monitored. “Thus, the results of that observational study are not necessarily in contrast to those of the present trial.”
My take: This type of study is difficult to complete. It is difficult to understand why exposure to cow’s milk in the first two weeks of life is helpful and why exposure in the first three days of life is detrimental with regard to the development of cow’s milk allergy.
*Katz Y, Rajuan N, Goldberg MR, et al. Early exposure to cow’s milk protein is protective against IgE-mediated cow’s milk protein allergy. J Allergy Clin Immunol. 2010;126(1):77-82.e1. doi:10.1016/j.jaci.2010.04.020)
Related blog posts:
Quebec City
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.