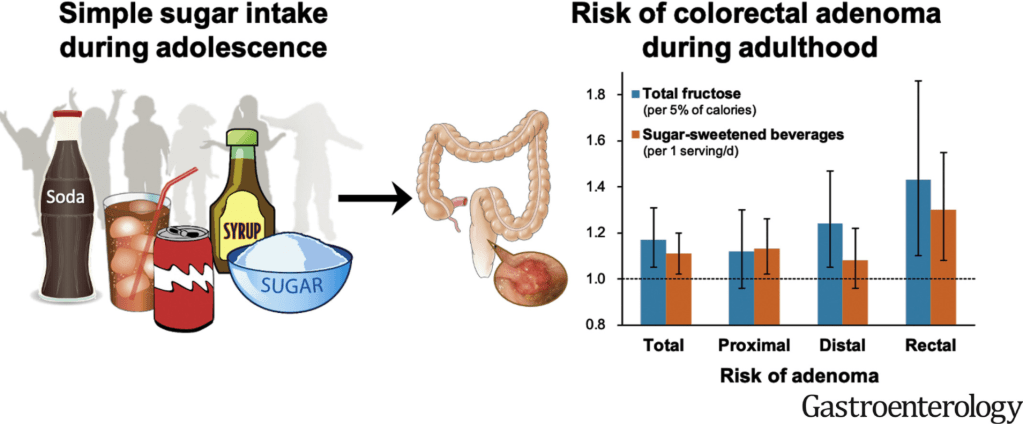
H-K Joh et al. Gastroenterol 2021; 161: 128-142. Full text: Simple Sugar and Sugar-Sweetened Beverage Intake During Adolescence and Risk of Colorectal Cancer Precursors
Methods: We prospectively investigated the association of adolescent simple sugar (fructose, glucose, added sugar, total sugar) and sugar-sweetened beverage (SSB) intake with CRC precursor risk in 33,106 participants of the Nurses’ Health Study II who provided adolescent dietary information in 1998 and subsequently underwent lower gastrointestinal endoscopy between 1999 and 2015.
Key Findings:
- High sugar and SSB intake during adolescence was positively associated with risk of adenoma, but not serrated lesions.
- Per each increment of 5% of calories from total fructose intake, multivariable ORs were 1.17 (95% CI, 1.05–1.31) for total and 1.30 (95% CI, 1.06–1.60) for high-risk adenoma
Full text (editorial, pg 27): JK Lee et al: Sugary Truth of Early-Onset Colorectal Neoplasia—Not So Sweet After All
Key points:
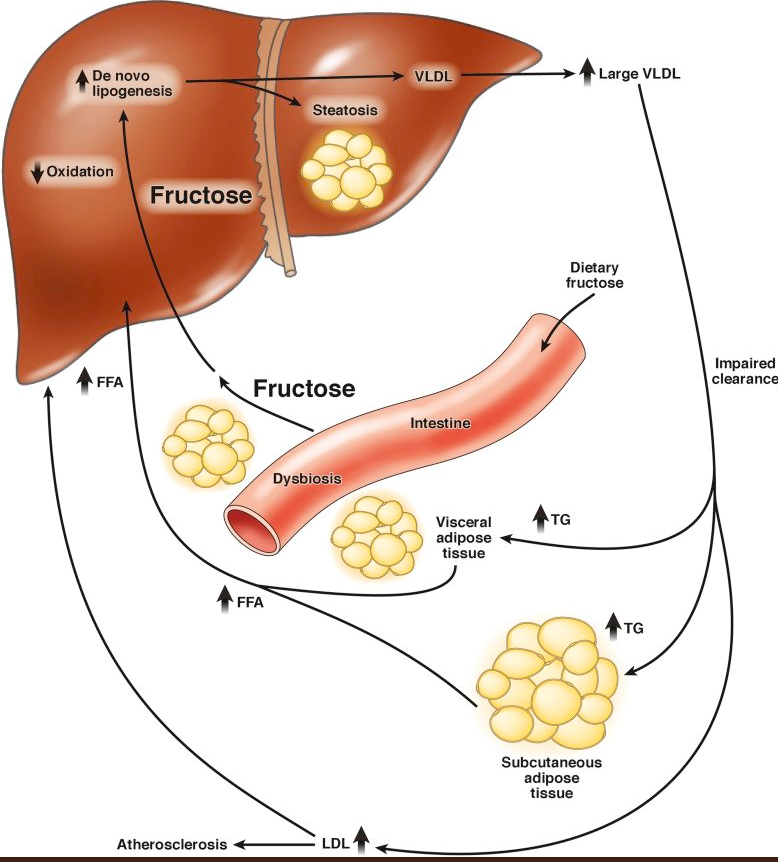
- “In the United States, SSB [sugar-sweetened beverage] consumption has increased by nearly 5-fold over time, from 10.8 gallons per person in 1950 to 49.3 gallons per person in 2000.8 In adolescents, SSB consumption has more than doubled since the 1960s and comprises the largest source of simple sugar and calories in their diets”
- “Recent studies, including several from the Nurses’ Health Study, have identified lifestyle factors from early adulthood, including Western diet,13,14 alcohol,15 tobacco,16 sedentary television viewing,11 diabetes,17 and obesity12 as risk factors for early-onset CRC or adenoma. Other studies report no association between sugar, fruit juice, and SSB consumption during adulthood and risk of CRC in older adults”
My take (borrowed from editorial): “Increasing fructose and SSB consumption, particularly among adolescents and young adults, is troublesome because substantial evidence links consumption to various health outcomes, including obesity, type 2 diabetes, cardiovascular disease, some cancers, all-cause mortality, and now early-onset high-risk adenoma…. clinicians should continue to support public health policies discouraging or reducing consumption of simple sugars and SSBs in adolescents, for whom exposure might have lifelong consequences.”