J Tobias et al. J Pediatr 2022; 244; 64-71. Open Access: Bifidobacterium longum subsp. infantis EVC001 Administration Is Associated with a Significant Reduction in the Incidence of Necrotizing Enterocolitis in Very Low Birth Weight Infants
Editorial: MA Underwood J Pediatr 2022; 64: 14-16. Open Access: Bifidobacterium infantis, Necrotizing Enterocolitis, Death, and the Role of Parents in the Neonatal Intensive Care Unit
Methods: Nonconcurrent retrospective analysis of 2 cohorts of 483 very low birth weight (VLBW) infants not exposed and exposed to B infantis EVC001 probiotic at Oregon Health & Science University from 2014 to 2020
Key findings:
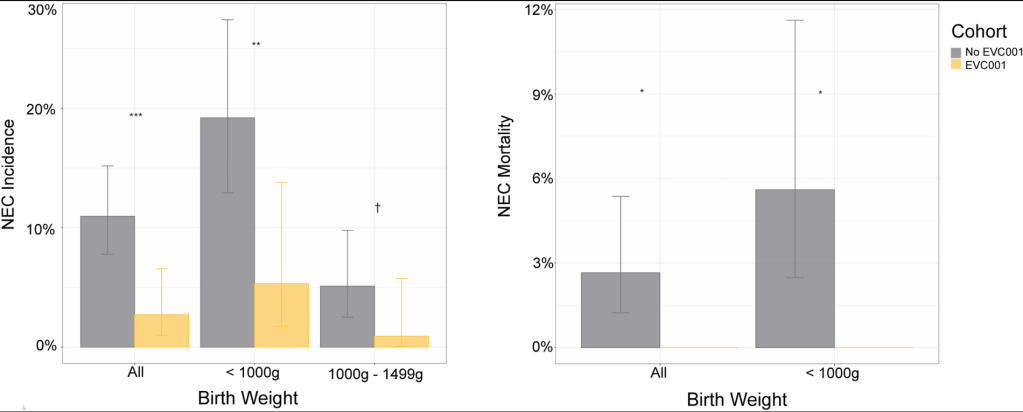
- The cumulative incidence of NEC diagnoses decreased from 11.0% (n = 301) in the no EVC001 (unexposed) cohort to 2.7% (n = 182) in the EVC001 (exposed) cohort (P < .01); this was a 73% risk reduction of NEC
- NEC-associated mortality decreased from 2.7% in the no EVC001 cohort to 0% in the EVC001 cohort (P = .03)
- There was a lack of adverse events (including probiotic sepsis)
Key points from editorial:
- “The first cohort study showing a significant decrease in necrotizing enterocolitis (NEC) with the routine administration of probiotic dietary supplements [was] more than 20 years ago”
- “The most recent Cochrane Database systematic review 2 included 56 randomized or quasi-randomized trials in which 10 812 infants participated. Meta-analysis found evidence for decreased risk of NEC (Risk ratio [RR] 0.54)”
- Both the AGA and ESPGHAN have recommended routine probiotics administration to preterm infants. However, the AAP recommends “against routine probiotic administration citing ‘the lack of FDA-regulated pharmaceutical-grade products in the United States, conflicting data on safety and efficacy, and potential for harm in a highly vulnerable population.’”
- “Recognizing that many neonatologists have opted to adopt routine probiotic administration to infants born preterm, the recent American Academy of Pediatrics statement6 recommends that an informed consent process for utilizing probiotics. Dr. Underwood counters: “there is no mention of a need to discuss these risks and benefits by those well-informed clinicians who may not believe that the data support administering probiotics. Inclusion of parents in decision-making in the NICU improves parent satisfaction and infant outcomes.”
- Parent and clinician resource: necsociety.org. 9 Things You Need to Know About Necrotizing Enterocolitis and NEC Facts
My take: It is hard to understand that, despite 20 years of research showing probiotics can reduce mortality and morbidity in premature infants, we have not been able to manufacture a consistent, reliable high-quality probiotic capable of meeting FDA standards.
