John Barnard MD gave a great talk today as part of the yearly Donald Schaffner lecture. This lecture also honored Larry Saripkin (see blog post: Thank You Larry) as a master clinician. My notes below may contain errors in transcription and in omission. Along with my notes, I have included many of his slides.
Key Points:
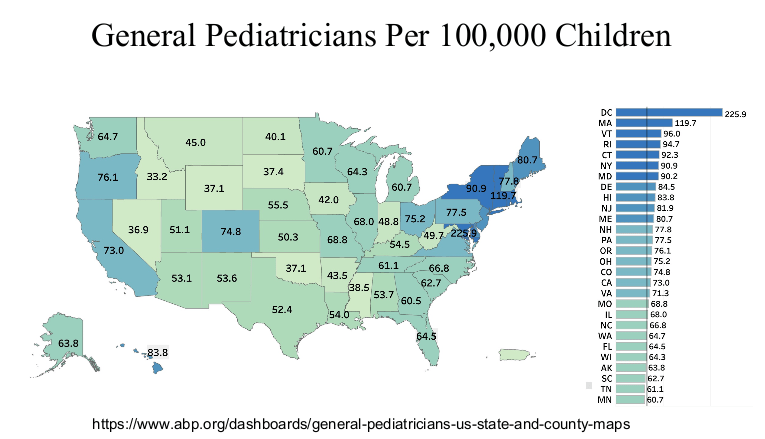
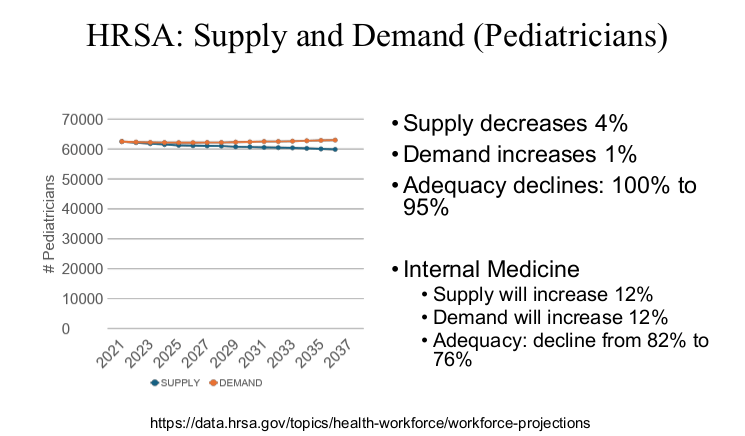
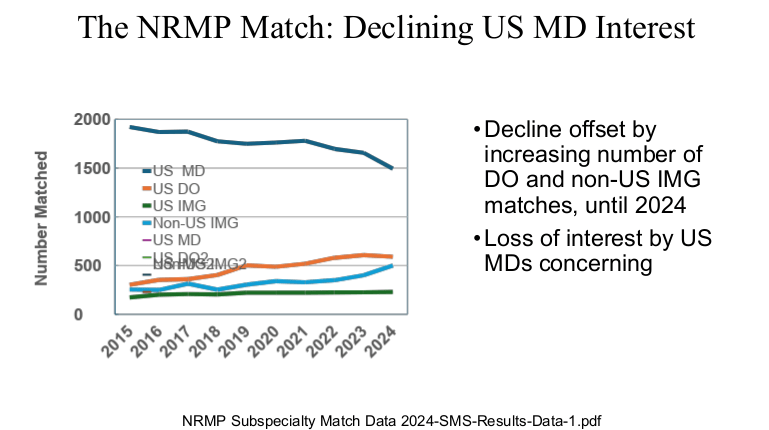
- Since 2015, there is less interest in U.S.-trained physicians to pursue a career in pediatrics.
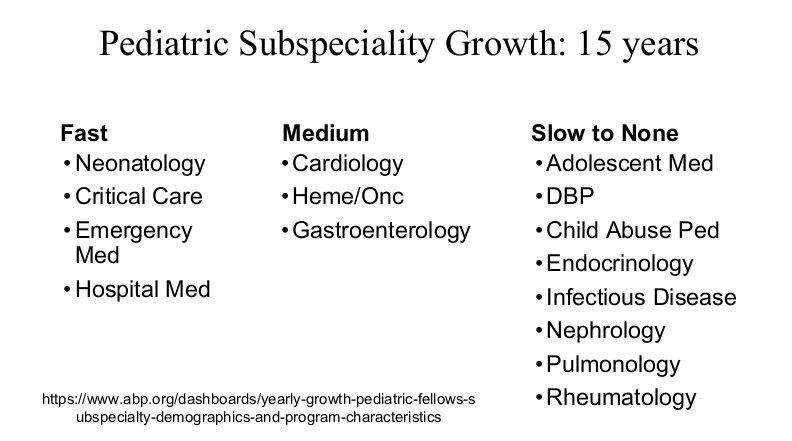
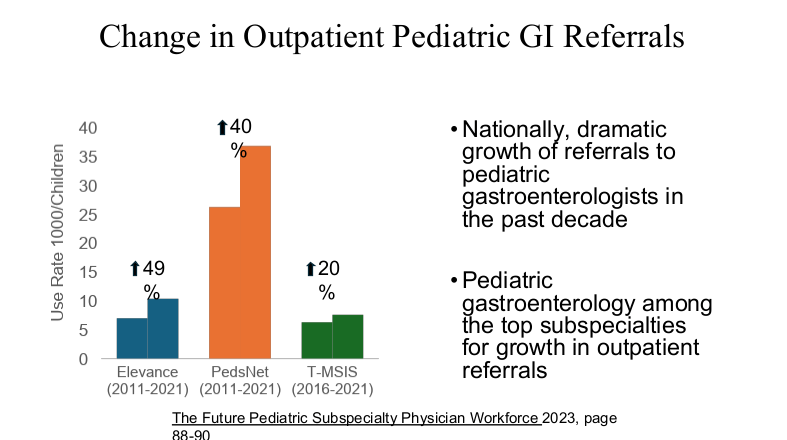
- The pediatric gastroenterology workforce continues to grow. Other pediatric subspecialties are understaffed and not attracting enough younger pediatric trainees
- The percentage of women and international medical graduates has been increasing; currently 67% of board-certified pediatricians are women and 22% are non-US international medical graduates
- Women through all medical fields and even in pediatrics segregate to less well-paying positions. For example, pediatric cardiology has a lower percentage of women and has a higher median income compared to many other pediatric subspecialty areas
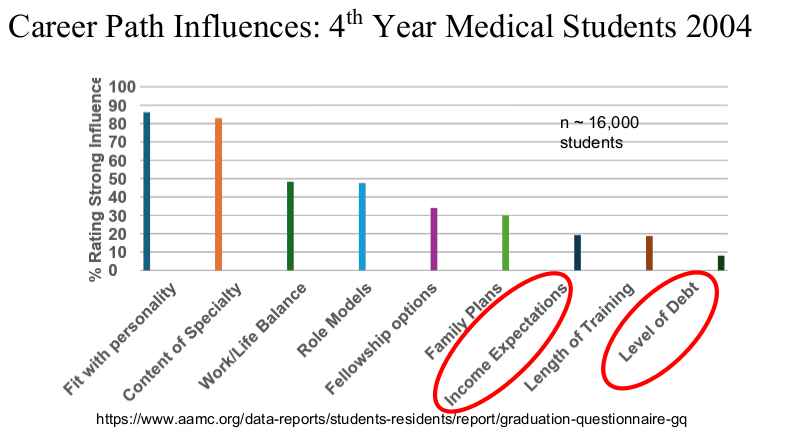
- While relatively lower pay is thought to be a driving force in choosing a career in pediatrics/pediatric subspecialty, several surveys of medical students indicate that this is not the only factor; other factors may be more important














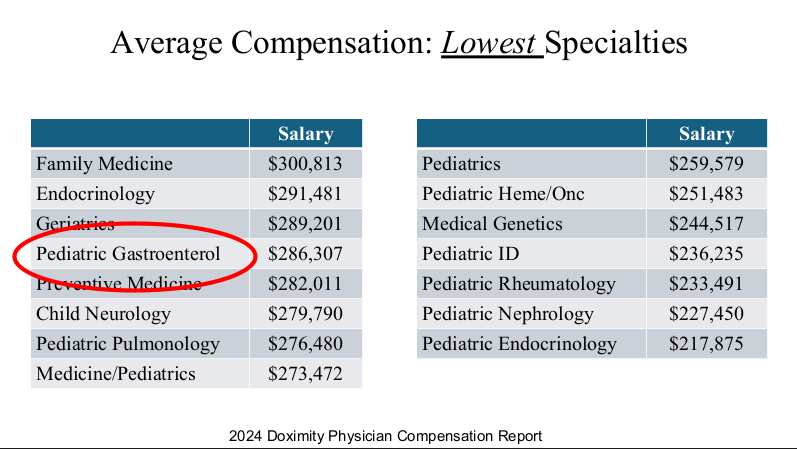
Physicians are in the top 5% of compensation, though pediatric physicians receive less
compensation than their peers. According to 2024 Doximity survey
(https://press.doximity.com/reports/doximity-physician-compensation-report-2023.pdf)
average physician salary exceeds $350,000 in most metro areas.



be a factor affecting physician job satisfaction




We need to make sure that our interests and the interests of children are heard.

My take: Dr. Barnard noted that “medicine has never been more exciting than it is today.” Yet, the decreased interest of medical students for a career in pediatrics/pediatric subspecialties needs to be addressed.
Dr. Barnard modified the material and presented the William Balistreri lecture at this year’s NASPGHAN meeting. Here are some additional slides from this talk which focused more on Pediatric Gastroenterology:


Related blog post: “Why It’s So Hard to Find a Pediatrician These Days”


