Recently, Dr. Laurie Jacobs from CHOA’s palliative care team gave our group a provocative update on communication strategies in children with severe illness. My notes below may contain errors in transcription and in omission. Along with my notes, I have included many of her slides.
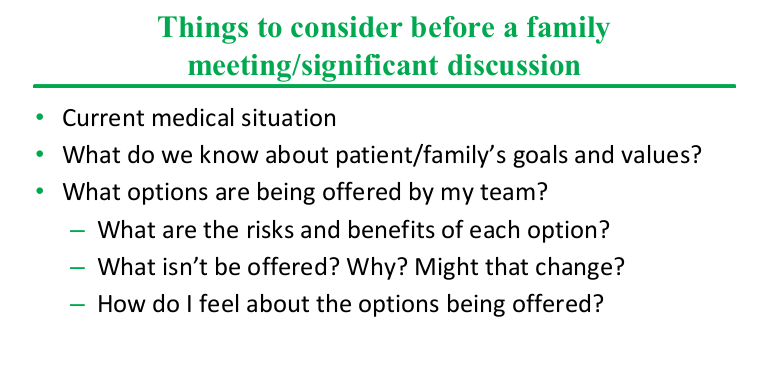
- Having a pre-meeting with other members of health care team is a key part in setting up an effective meeting with parents
- Delivering news: 1) Provide a straightforward Headline: ‘We are here to discuss xyz’ 2)Be clear. ‘To be clear is to be kind’ 3) Then STOP TALKING. This let’s the family process
- Sometimes even delivering bad news can be met with relief by families who have been waiting for a diagnosis
- Respond to emotion with NURSE mnemonic: Name, Understand, Respect, Support, Explore
- What if the ‘family doesn’t get it?’ Do they understand (can they repeat back)? Most often the family has a different perspective; they may think we are wrong
- Be careful to avoid offering decisions where there are not actual decisions to be made
- Our own values/beliefs are often introduced even though quality of life is in the eye of the beholder
- Tube feeds can be considered forms of ‘artificial nutrition.’ There are situations in which families need to know that it is not always required
- Parenteral nutrition is more invasive and associated with more active parental decision-making
- Decisions may change based on change in patient circumstances
- There is not a single right answer with difficult decisions. There are trade-offs between longevity and QOL
- Anything that we would allow parents not to start, can be stopped at any time from an ethical standpoint











Related blog posts:
- Home Parenteral Nutrition in Children with Severe Neurological Impairment
- Trisomy 18 Trends over the Last 20 Years
- How Parents Feel After Tracheostomy Decision
- Pain in Children with Severe Neurologic Impairment
- Short Bowel Syndrome is a Full Time Job
- Personal Account of Extreme Short Bowel Syndrome (with Jeff Lewis)
- “Do Unto Others”
