AL Kilgore et al. JPGN 2024; https://doi.org/10.1002/jpn3.12390. Open Access! Evaluation and management of pediatric refractory constipation: Recommendations from the NASPGHAN neurogastroenterology and motility committee
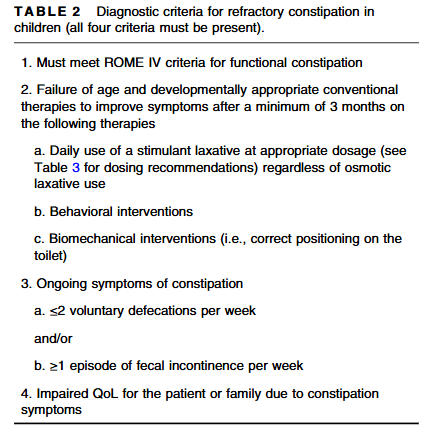
Selected Recommendations:
Evaluations:
- Screen for thyroid disease and celiac disease (though acknowledges that the data regarding an association between celiac disease and constipation are inconsistent)
- The use of an AXR in RC should be reserved for those patients unable to provide a reliable medical history and/or unable to allow for a physical exam (including a DRE), or to evaluate for mechanical obstruction or colonic distention when considering surgical interventions
- A contrast enema (CE) can be used to screen for HD or to assess colorectal anatomy
- There is no evidence to recommend the routine use of defecography in children
- Abdominal ultrasound has a good agreement with digital rectal exam (DRE) to evaluate for fecal impaction but should not be performed in place of DRE
- ARM should be used to screen for the presence of a RAIR. If anal spasms and prolonged sphincter relaxation are detected during ARM, an assessment for spinal abnormalities can be considered
- An LS MRI should be performed in pediatric patients with RC associated with physical or neurological signs of spinal anomalies, signs of neurogenic bladder on urodynamics, or when the anorectal manometry (ARM) is abnormal suggesting spinal cord abnormalities
- Colonic transit time (CTT) via radiopaque markers should be completed for patients with RC with equivocal medical history and to screen for the need to perform colonic manometry (CM)
- Colonic manometry (CM) should be performed only after medical therapy has been exhausted and surgical therapy is being considered. CM should be used to guide the timing and type of surgery to address RC. CM should be used to guide when to perform an ostomy takedown
- Rectal biopsies should not be used routinely in patients with RC and are indicated exclusively in patients with a suspected diagnosis of HD
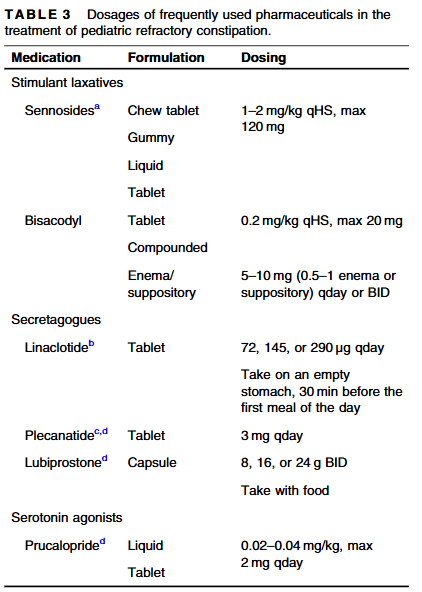
Pharmaceuticals:
- High-dose sennoside (or Bisacodyl) is a mainstay of management of RC and should be optimized for the individual patient before considering further management options
- A secretagogue (or prucalopride) should be considered as an adjunct to a high-dose stimulant laxative when treating RC with poor response to optimized high-dose stimulant laxatives or when high-dose stimulant laxatives are not tolerated
- There is no clear role of anal botox in the treatment of patients with RC without a diagnosis of IAS achalasia
- Early intervention with daily stimulant laxatives in the treatment of FC is encouraged to try to prevent the disease progression from functional constipation (FC) to RC
- Antegrade and Retrograde Treatments:
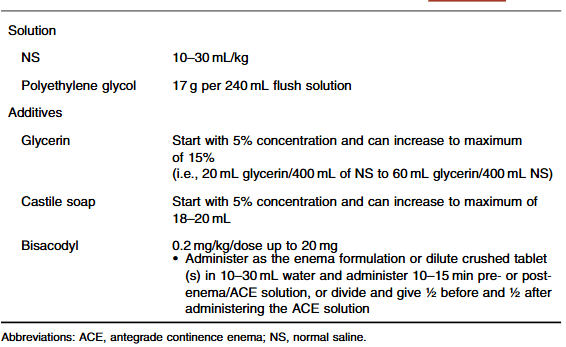
- The last part of the recommendations include antegrade continence enemas, surgical approaches, and complicated algorithms (see Figure 1 and Figure 2)
My take: These recommendations address a widespread problem for pediatric gastroenterologists and are useful for those with and without an interest in motility disorders.
Related blog posts:
- ANMS Virtual Symposia on Constipation
- Pictographic Constipation Action Plan
- New Data on Bisacodyl for Pediatric Constipation
- Safety of Senna-Based Laxatives
- Constipation Action Plan: Better Instructions, Fewer Phone Calls
- Does It Make Sense to Look for Celiac Disease in Children with Functional Constipation?
- You Can Do Anorectal Manometry in Your Sleep, But Should You?
- More than Two Years of Constipation Before Specialty Help
- NASPGHAN Postgraduate Course 2017 (Part 5): Refractory constipation, Extraesophageal GERD, POTS, Recurrent Abdominal Pain
- Refractory Constipation -Terrific Update
- How Sensory Processing Contributes to Constipation in Children
- Is There a Residual Impact of a Tethered Cord on Colonic Motility
- AGA Constipation Guidelines
- Radiographs and Constipation -Bad Practice and Good Study
- Quality Improvement: Fewer Xrays for Constipation
- Long Term Use of Polyethylene Glycol (PEG 3350)
- Is It a ‘Waste’ to Do Colonic Manometry in Kids with Autism?
- Reliability of colonic manometry
- Useful (Open Access) Reference for Colonic Motility Studies
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.
