Eric Topol has summarized some of the recent advances in the understanding of the Gut-Brain Axis. Open Access Link: The Gut-Brain Axis Takes Center Stage (6/22/25)
Here’s a lengthy excerpt:
We’ve known about the gut-brain axis for decades but there has recently been an unprecedented jump in our knowledge base that has transformed our expectations for its preeminence.
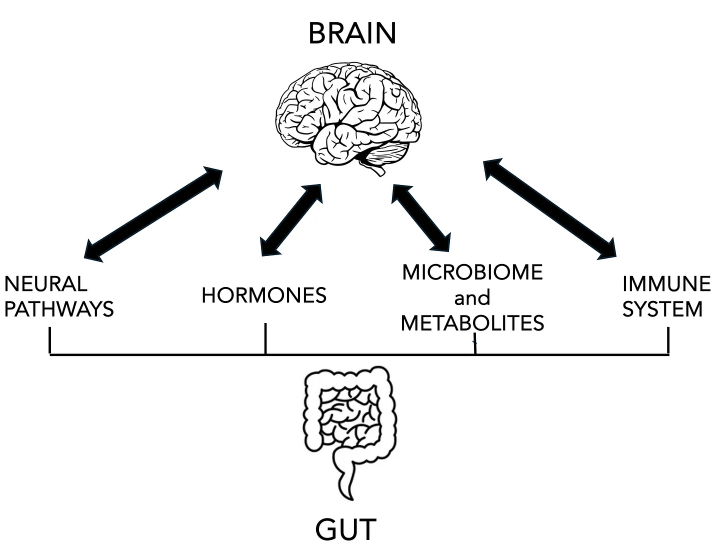
There are 2 types of neural pathways, the “second brain” referring to the enteric (gut) nervous system from the cells that line the intestine and communicate to the vagus nerve to the brain (and in the opposite direction, too). There are also connections via the sympathetic, parasympathetic nervous system (autonomic nervous system, ANS) branches and spinal cord innervation to the gut primarily through the ANS.
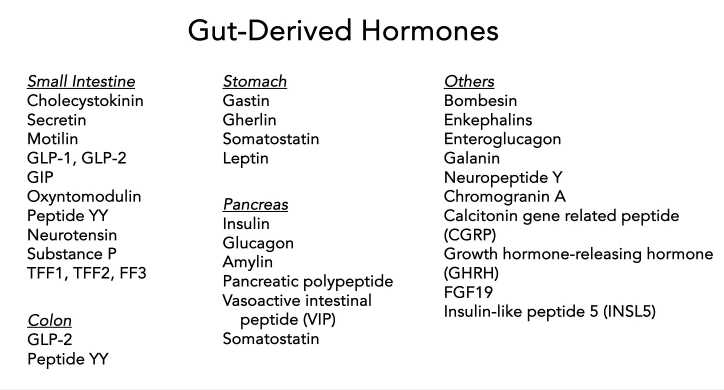
Cells in the gut produce hormones (enteroendocrine cells) such as glucagon-like peptide (GLP-1), gastric inhibitory peptide (GIP), peptide YY, secretin, gherlin, gastrin, and many others. Some of these regulate pancreatic hormones such as insulin, glucagon and amylin, which can be considered as gut hormones but derived from pancreatic cells rather than intestinal lining cells. The hormonal interaction between gut and brain also goes through the hypothalamus-pituitary-adrenal (HPA) axis.
The abundant and diverse bacteria in the gut microbiome of tens of trillion of cells of more than 3,000 species. These gut bacteria and their metabolites have an outsized impact by producing or stimulating different neurotransmitters (5HT, GABA) and metabolites (e.g. short chain fatty acids, SCFAs) that communicate with the brain and the immune system. For example, see my previous Ground Truths on how a gut bacteria and its metabolites can drive sugar cravings.
The interaction with the immune system is critical to maintain integrity of the gut lining (avoiding “leaky gut syndrome”) and the blood-brain-barrier…
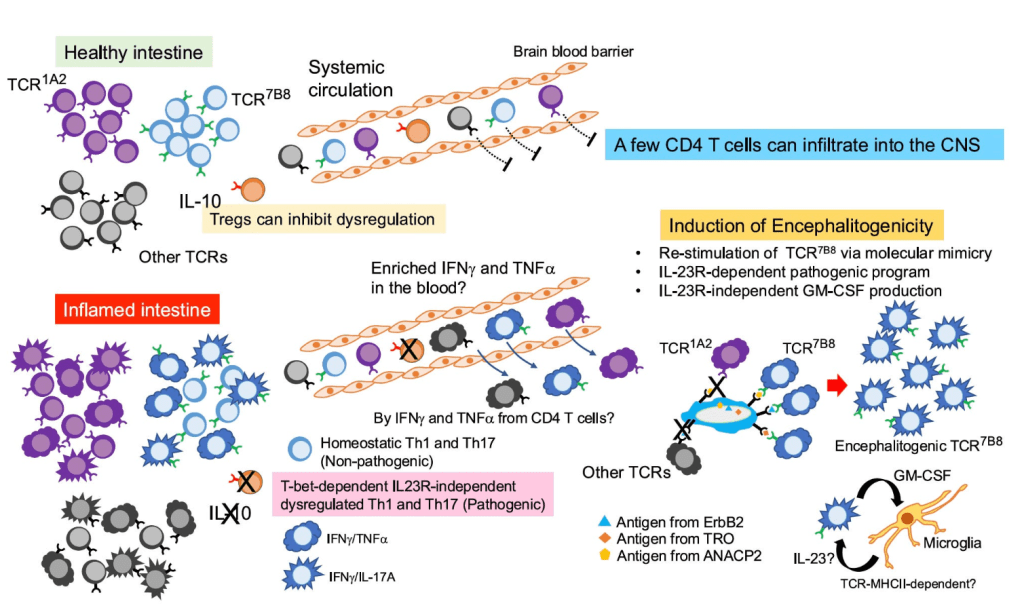
The precise way by which the gut can induce inflammation in the brain has remained unclear. In the journal Nature this week it was shown that inflamed gut-derived CD4+ T cells can infiltrate the brain, leading to neuroinflammation and neurological damage in the experimental model…bacteria derived proteins (antigens) looking like host derived proteins, inciting an immune response.
This was the second of 2 recent discoveries centered around gut-derived immune cells that get into the brain. Newly identified specialized CD4+ T cells from the gut and white adipose tissue establish residence in the brain’s subfornical organ and regulate feeding behavior…
It turns out the H. pylori can do good things too! As in blocking the formation of amyloid protein formation. This week in Science Advances it was demonstrated that H. pylori releases the protein CagA (cytotoxin-associated gene A) which potently inhibits pathogenic amyloid assemblies..for formation in Alzheimer’s disease, Parkinson’s disease and type 2 diabetes…
Several new gut hormone clinical trials, beyond the ones that are widely used—semaglutide (Ozempic) and tirzepatide (Zepbound, Mounjaro), were unveiled…Through randomized trials, their broad impact has been unequivocally proven for diabetes, obesity, and for treating related conditions of heart failure (with preserved ejection fraction), kidney disease, liver disease, sleep apnea, along with unexpected suppression of addiction to alcohol, cigarette smoking, nail biting and gambling. Add a surprising impact that we’re starting to see for autoimmune diseases. Even before there is weight loss with these drugs, there is evidence from experimental models of reduced systemic (body-wide) and brain inflammation. What is surprising is that drugs like semaglutide have little direct penetrance to the brain, but exert their effect chiefly through the gut-brain axis. New molecules in this class will have enhanced brain penetrance…
Will They Work For Alzheimer’s Disease?
[In a Liraglutide trial with 200 participants with Alzheimer’s,] after 1 year of treatment there was a reported 18% less cognitive decline and 50% reduced brain shrinkage compared to placebo…[There are also two studies] pending EVOKE and EVOKE Plus trials of daily oral semaglutide participants aged 55–85 years with mild cognitive impairment or mild dementia due to Alzheimer’s…About 12% of American adults are already taking GLP-1 drugs