Recently Dr. Bezerra gave our group a terrific lecture. I have taken some notes and shared some of his slides. There may be inadvertent omissions and mistakes in my notes. In addition, Dr. Bezerra’s presentation included several lengthy animations which helped explain the basic science concepts. These are not included in this summary.
Prior to his presentation to our group, Dr. Bezerra’s accomplishments had been recognized with the Shwachman Award, the highest honor bestowed by our national pediatric GI organization NASPGHAN (NASPGHAN Awards 2025). On a personal note, Jorge was the first person to give me hands-on instruction with an endoscope and I have a great deal of admiration for his humility, thoughtfulness and scientific achievements.
.
Key points:
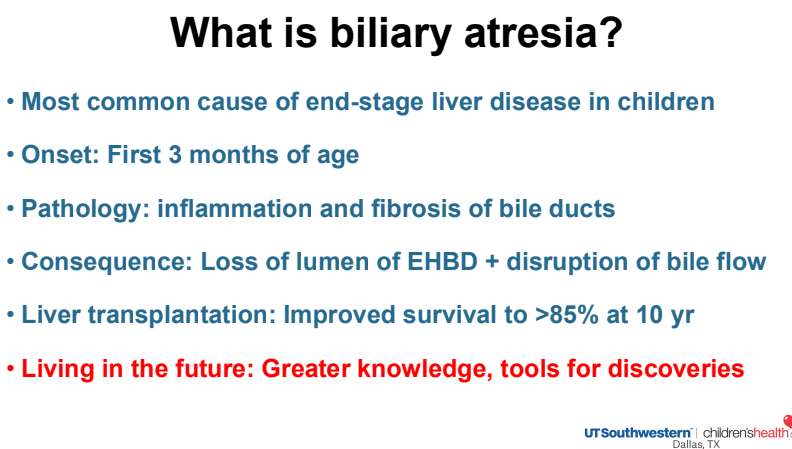
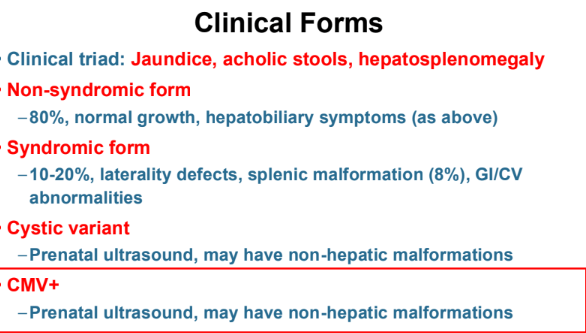
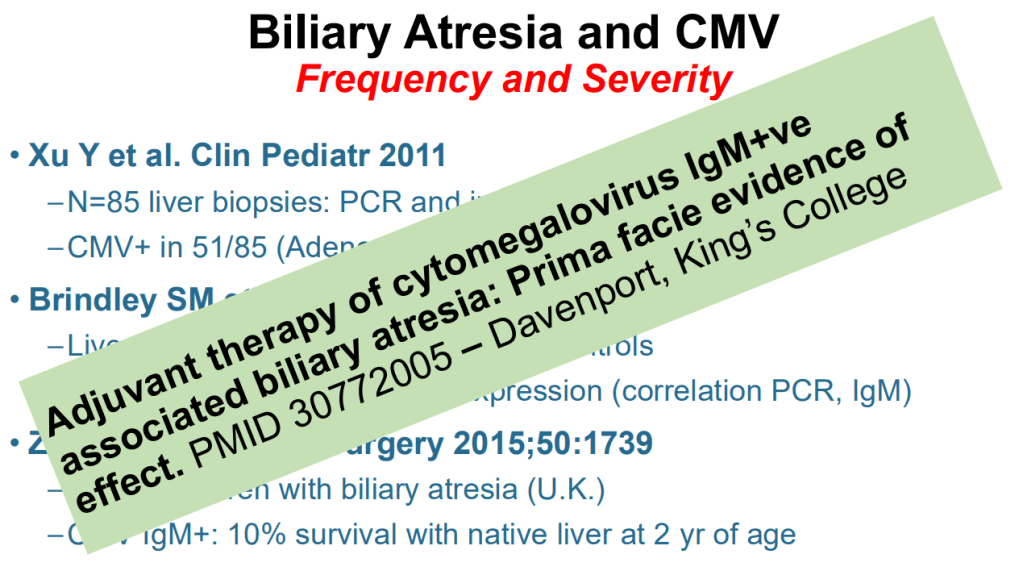
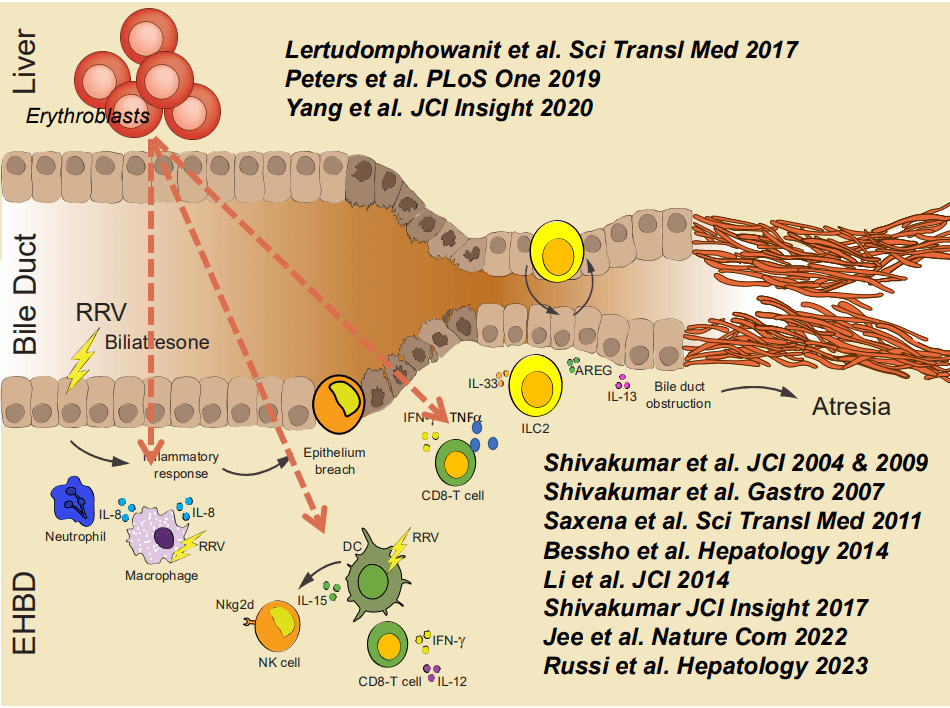
- Cytomegalovirus (CMV) is frequently associated with biliary atresia (BA). Treatment of CMV when detected may improve outcomes
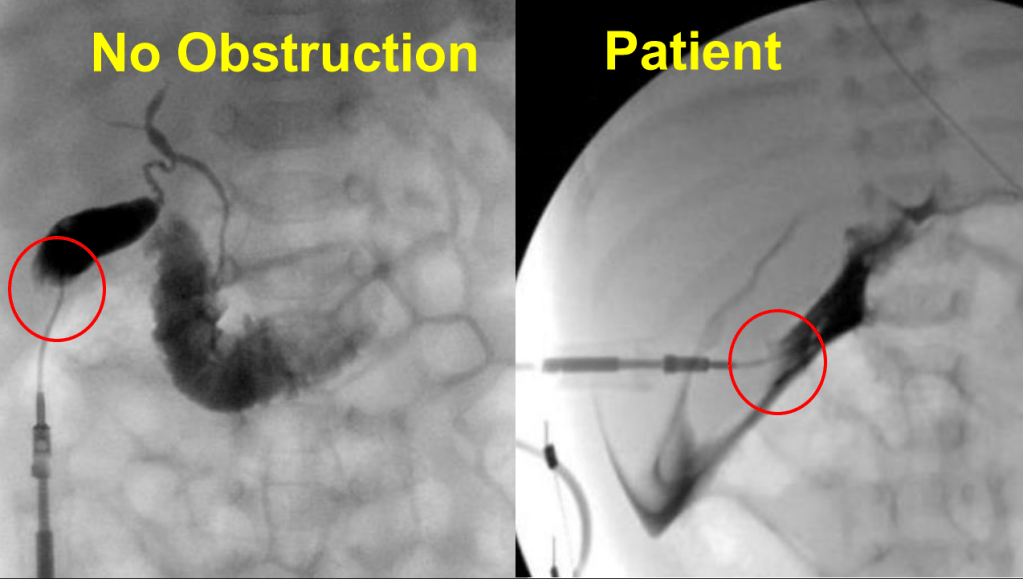
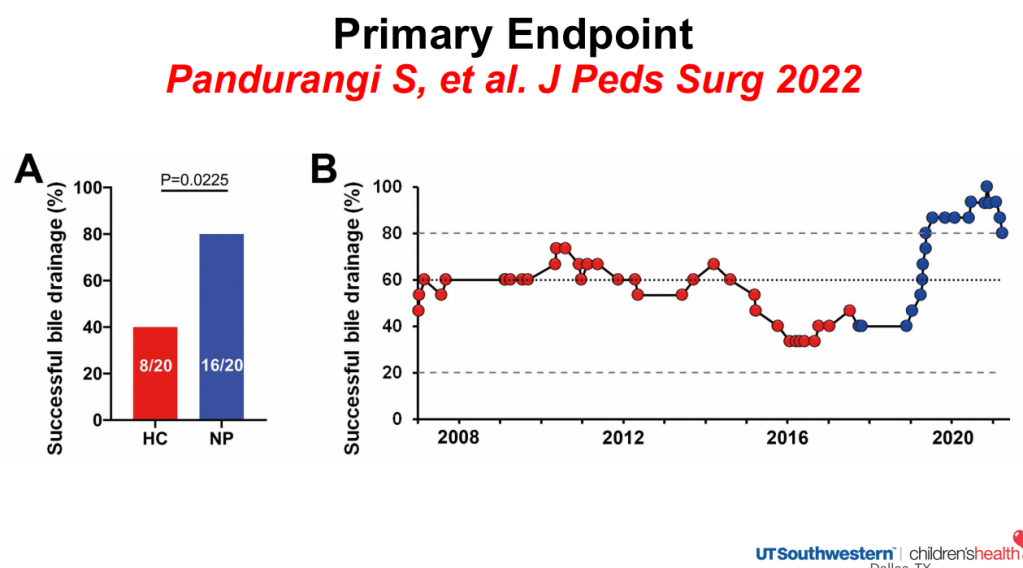
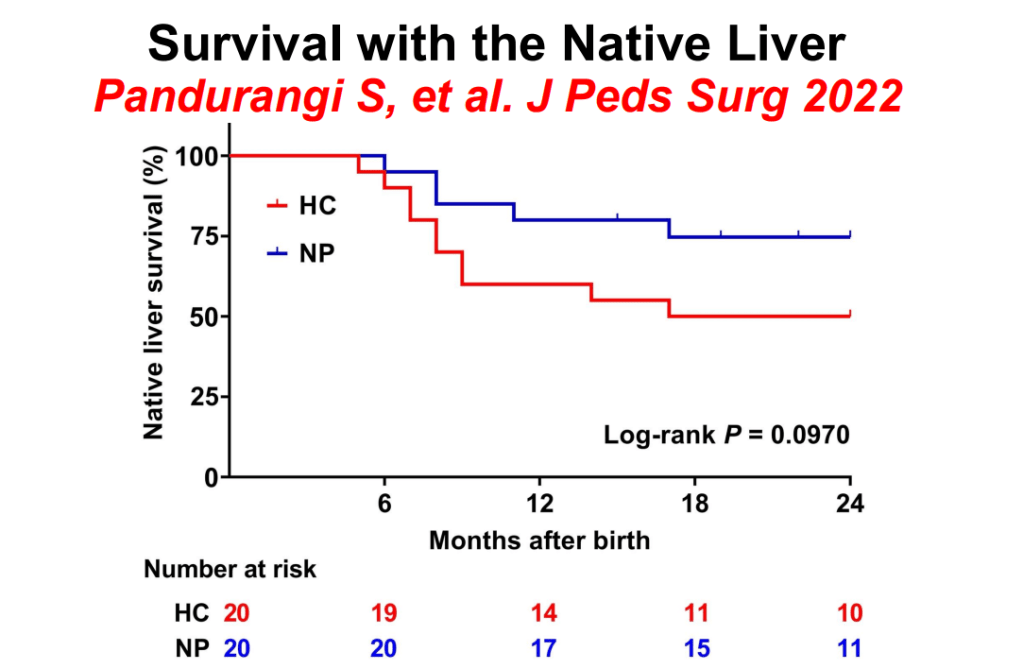
- Hepatoportoenterostomy (HPE) (aka Kasai procedure) is effective in about half of patients. The remainder develop complications that include recurrent cholangitis, portal hypertension, and cirrhosis which may lead to the need for liver transplantation
- 10-year survival rates for liver transplantation are >85%.
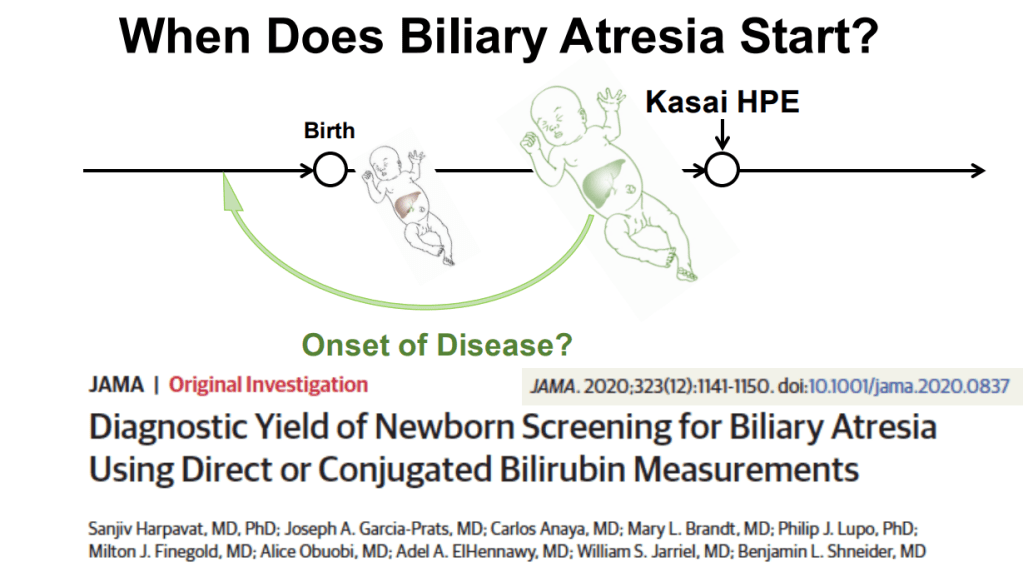
- There is now strong evidence that BA starts prior to birth as elevated conjugated bilirubin levels labs are detectable in the first 48 hours of life (related posts: Landmark Study on Universal Screening for Biliary Atresia -It Works!, Identifying Biliary Atresia in Infants: New Guidelines)
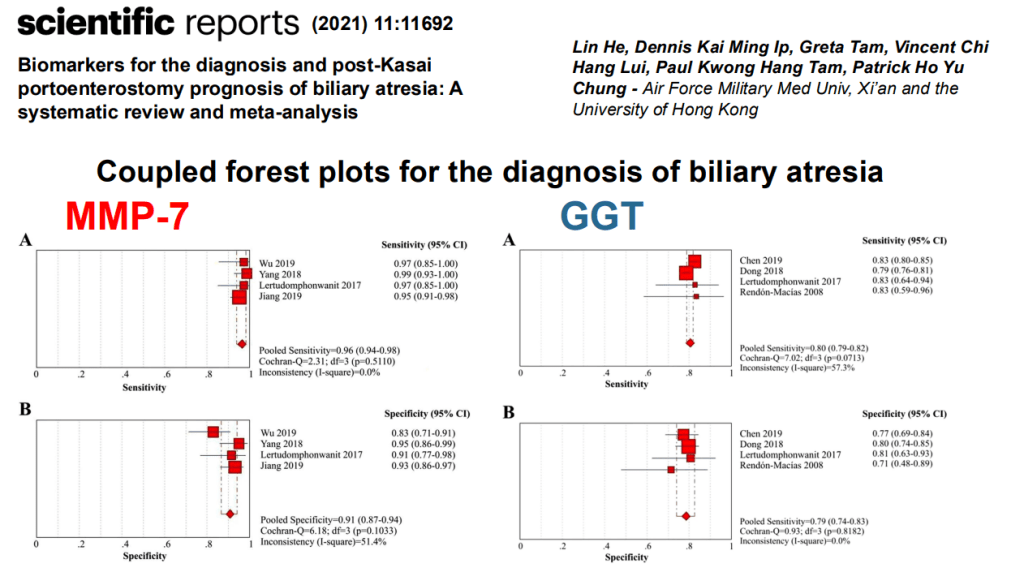
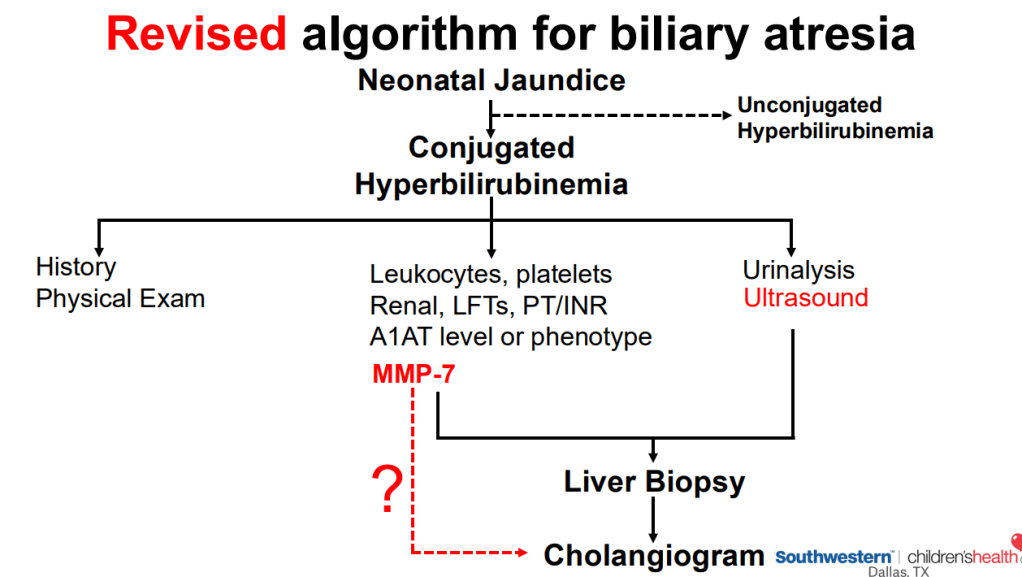
- MMP-7 and GGT can help predict the likelihood of BA
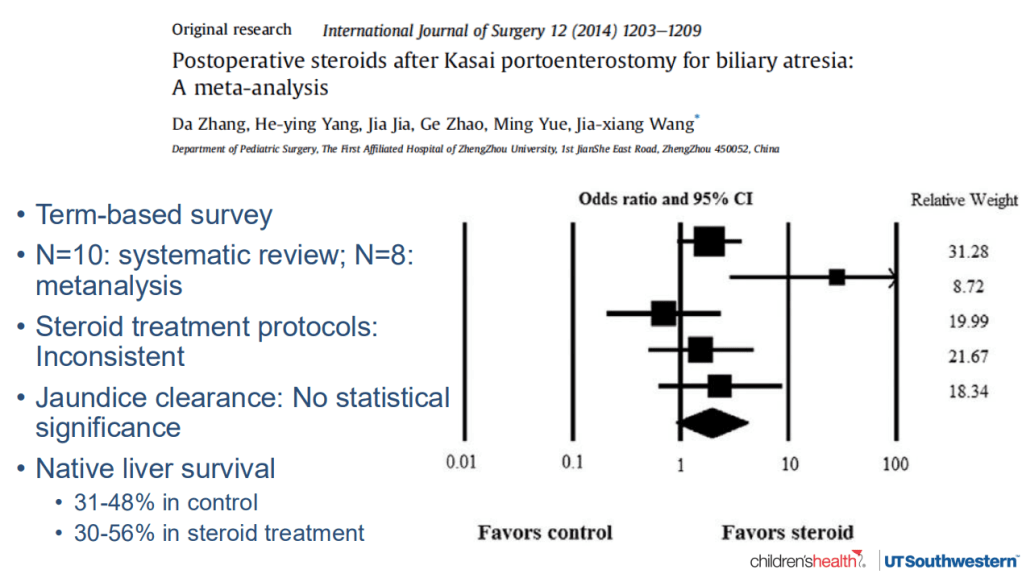
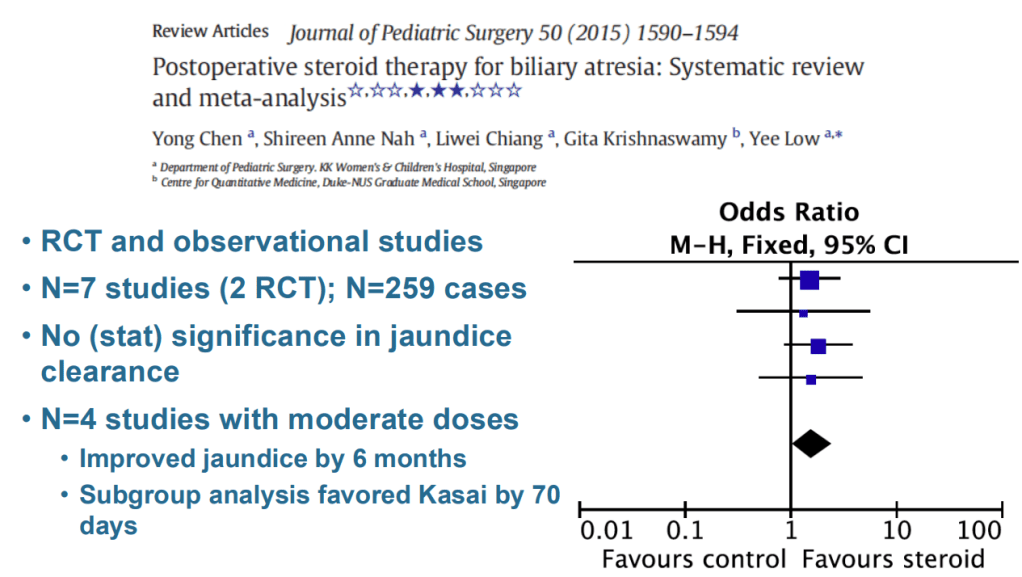
- Following HPE, there has been conflicting information about the utility of steroids to improve outcomes. A large randomized study (the START trial) (related post: START Study: Steroids Not Effective For Biliary Atresia (After Kasai)) found no difference in outcomes
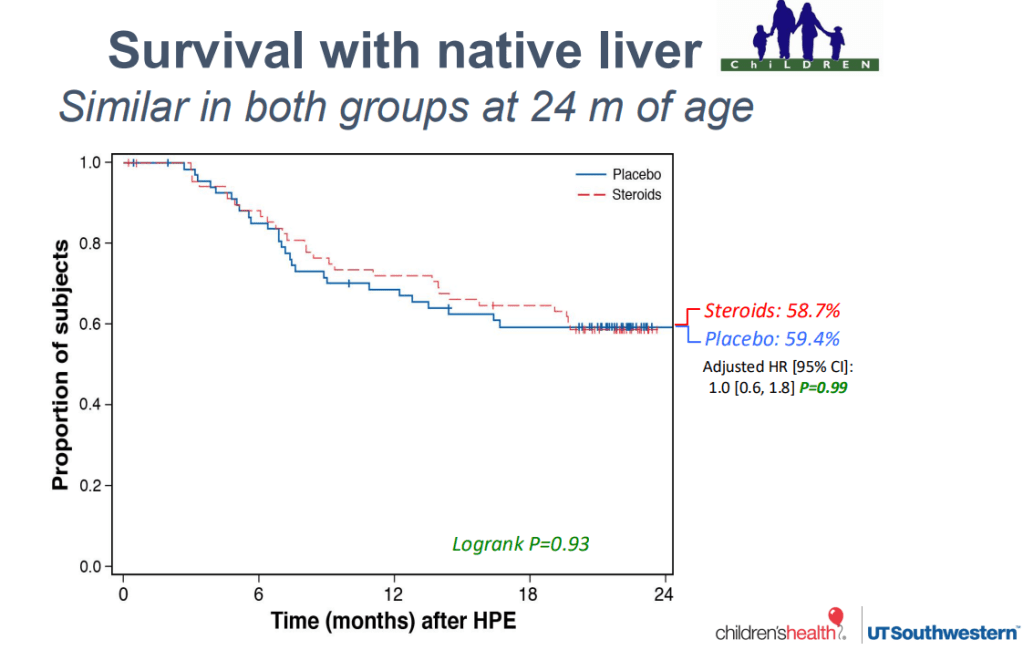
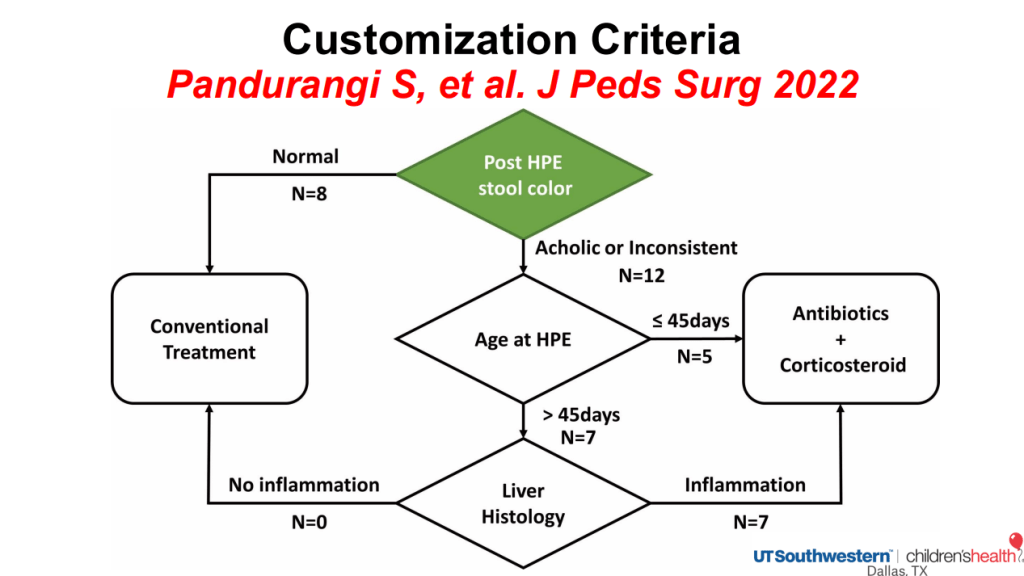
- However, many observational studies indicate that there may be some benefit (related post: Customized Postoperative Therapy for Biliary Atresia -Does It Help?)
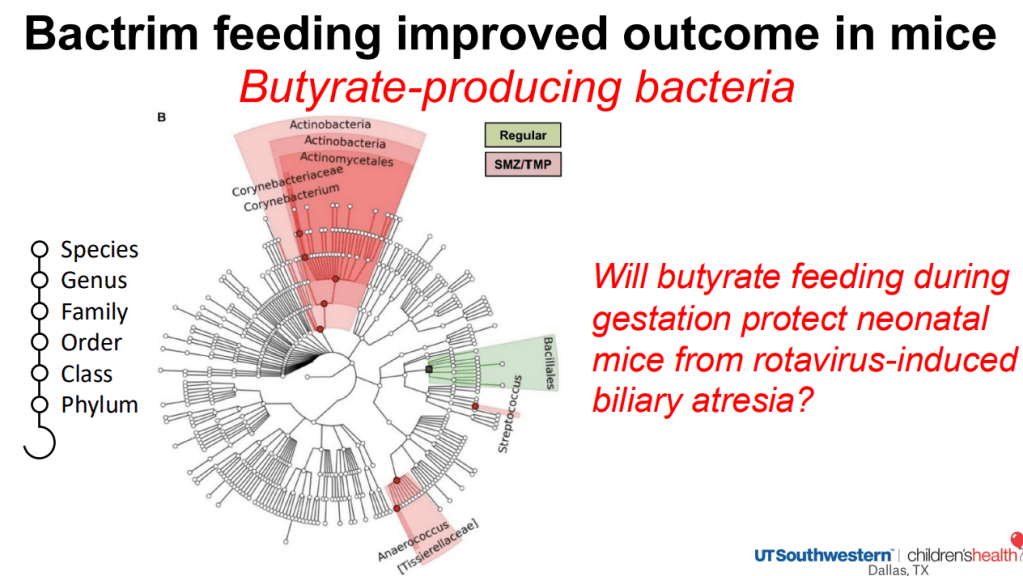
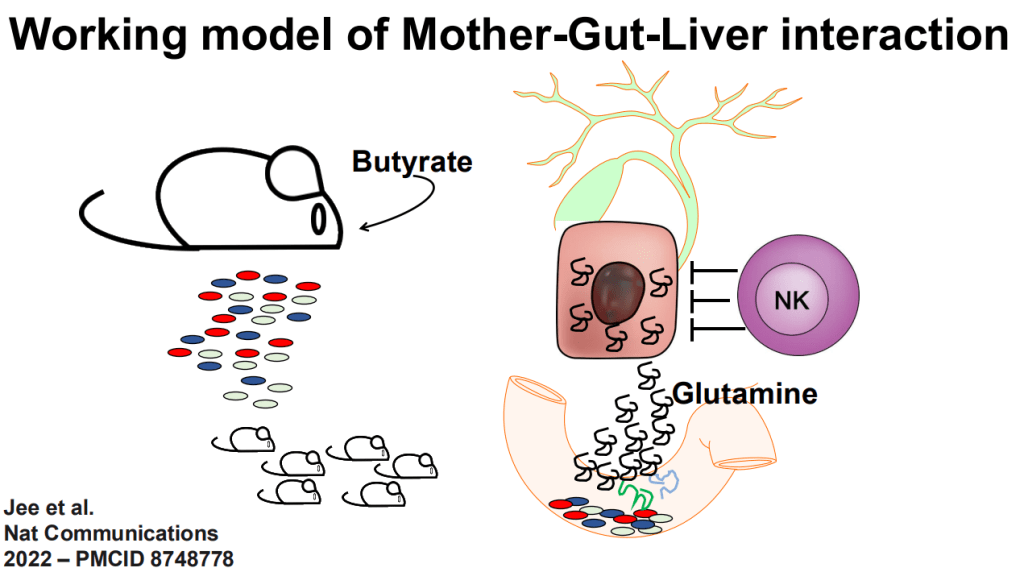
- The role of the microbiome is being explored as a factor in the predisposition to BA
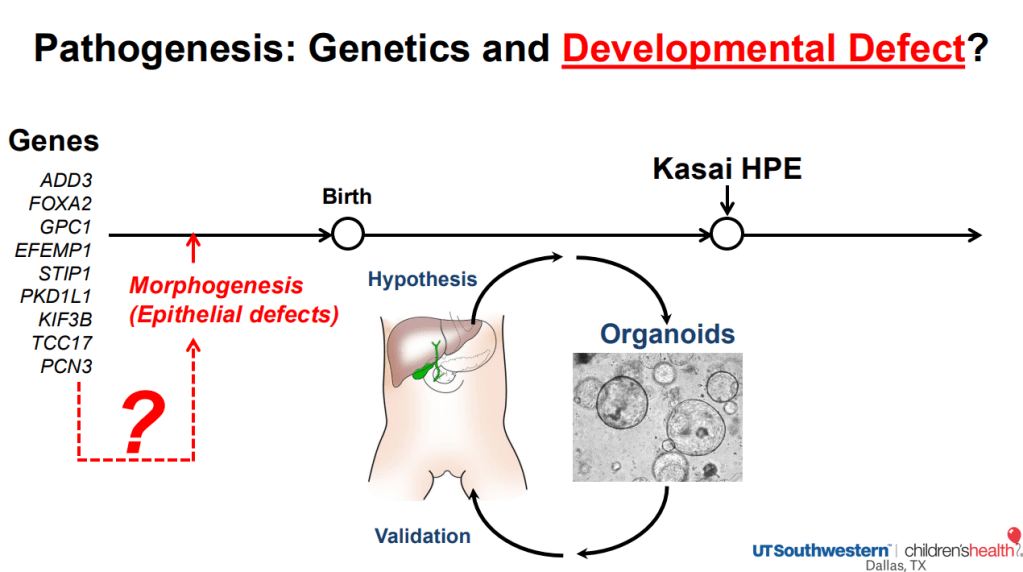
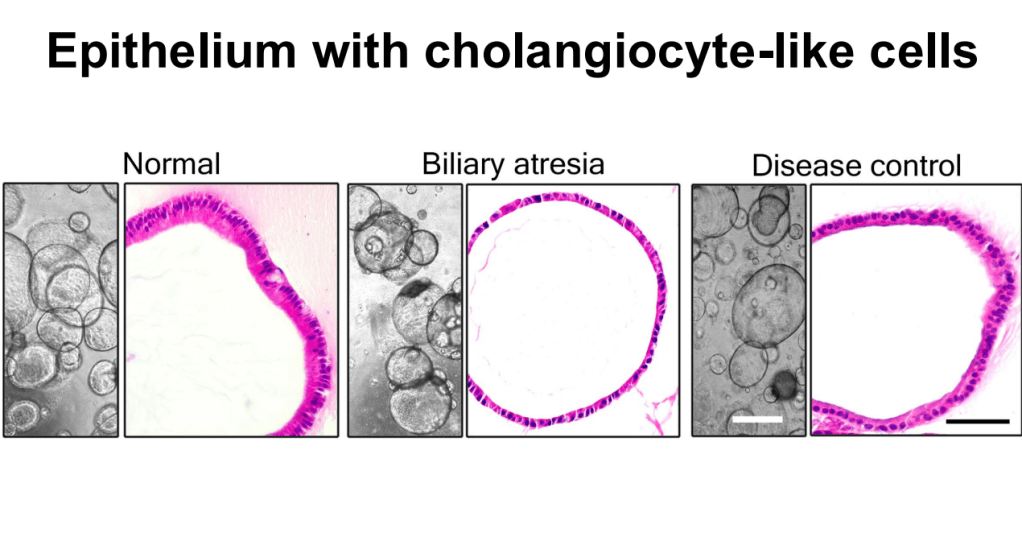
- Biliary atresia organoid studies: Biliary atresia organoids had decreased expression of genes related to EGF signaling and FGF2 signaling. When treated with EGF+FGF2, biliary atresia organoids expressed differentiation markers, which restored polarity (Reference: Hepatology 2022 Jan;75(1):89-103. doi: 10.1002/hep.32107. Biliary organoids uncover delayed epithelial development and barrier function in biliary atresia). Thus, these organoids can help understand the underlying pathogenesis and may lead to improved treatments
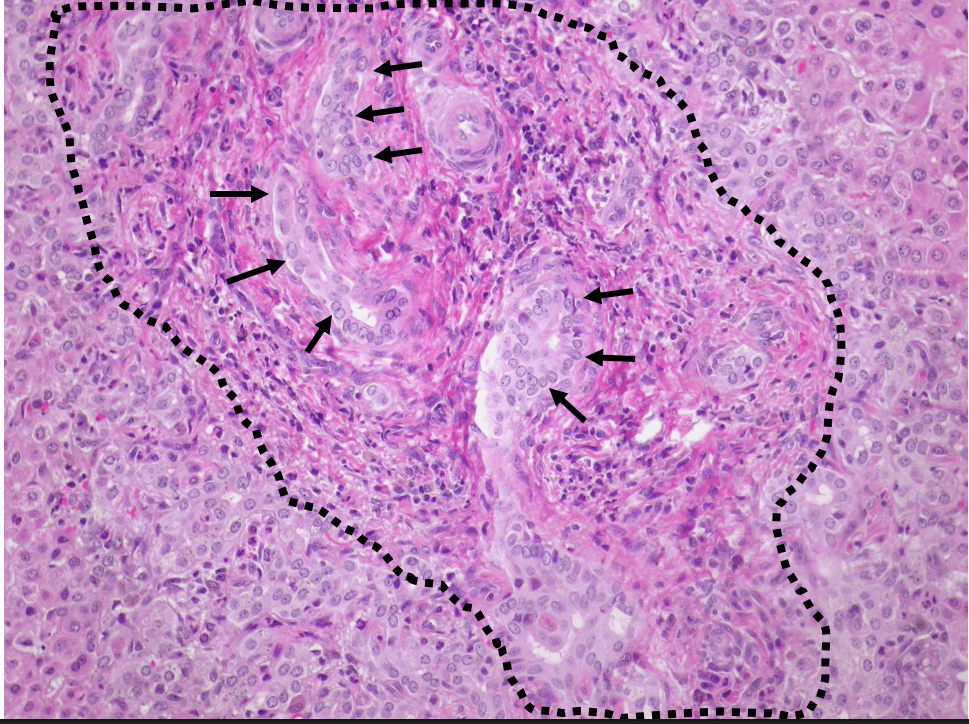
- More recently, compared to normal liver organoids, the epithelium of BA organoids was fragmented and peribiliary glands (PBGs) were small, had abnormal intercellular junction (ZO1 expression), and expressed markers of epithelial-mesenchymal transition (EMT), with a prominent expression of TGF-β3. Upon TGF-β inhibition, EMT decreased in the diseased epithelium, the population of PBGs increased, and ZO1 expression improved. In vivo, TGF-β inhibition suppressed the BA phenotype and substantially decreased liver fibrosis in neonatal mice. Thus, the modulation of TGF-β-dependent EMT regulates bile duct epithelial development and influences the susceptibility of neonates to biliary injuries. (Reference: Nat Commun 2025 Jul 17;16:6575. doi: 10.1038/s41467-025-61442-5. Open Access! Cellular crosstalk mediated by TGF-β drives epithelial-mesenchymal transition in patient-derived multi-compartment biliary organoids)
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition
