Mary Suhr, a coding expert, provided our group with an excellent update on coding and the changes needed in documentation. I have taken some notes and shared some of her slides. There may be inadvertent omissions and mistakes in my notes.
- In 2025, billing/coding relies entirely on medical decision-making OR time codes. While documenting a comprehensive history and an exam are important for patient care and good practice, they are not important in billing/coding.

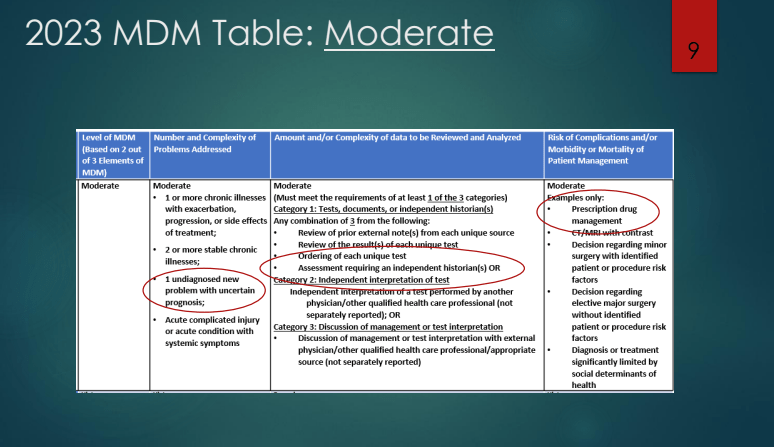
- Medical decision-making (MDM) consists of three areas: diagnosis, review of data, and risks of treatment. Data includes points for each lab reviewed/ordered and each radiology test. If you order/review CBC/d, CRP, and CMP, this would be up to 3 points in this category.

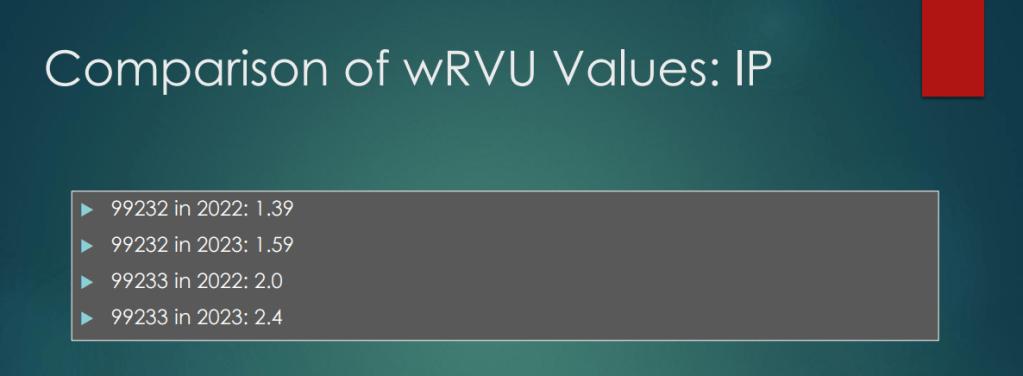
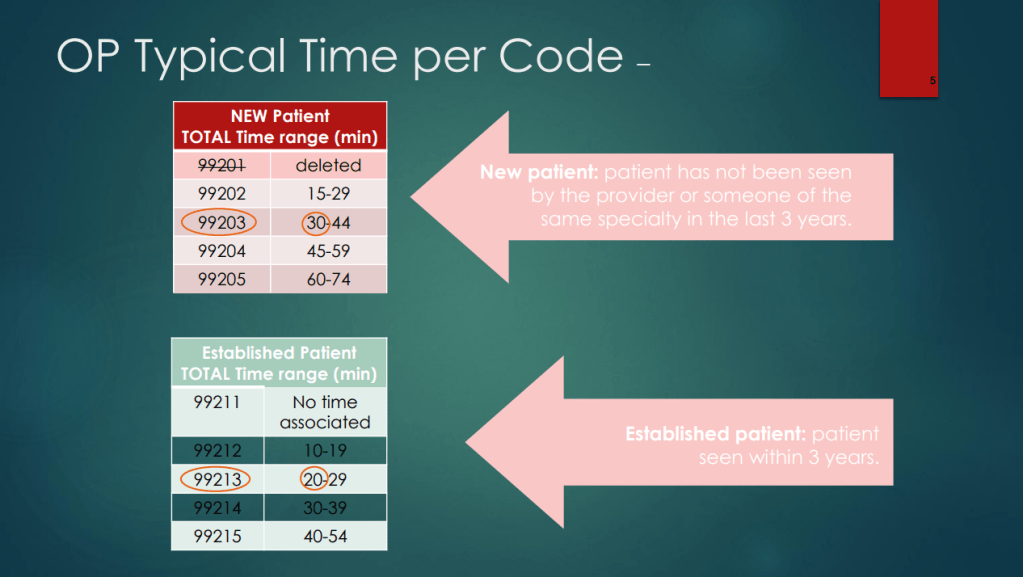
- With the changes in requirements in coding, the RVUs were increased for both outpatient and inpatient codes. This reflects the increased difficulty in selecting some codes. For example, the change in requirements, some 99214 codes several years ago will now qualify for 99213 codes. It is much more difficult to use a 99215 code based on medical decision-making and the time spent is up to 40 minutes to use this code

- Followup visits who are not doing well generally would NOT be a low level visit if documented appropriately



or the MD can bill based on medical decision-making (but not time code).

- Discontinuing a prescription medication can be counted as prescription drug management if documentation explains the potential benefits/risks of this
- Newer codes that may be useful:
- G2211 –>long-term longitudinal care code
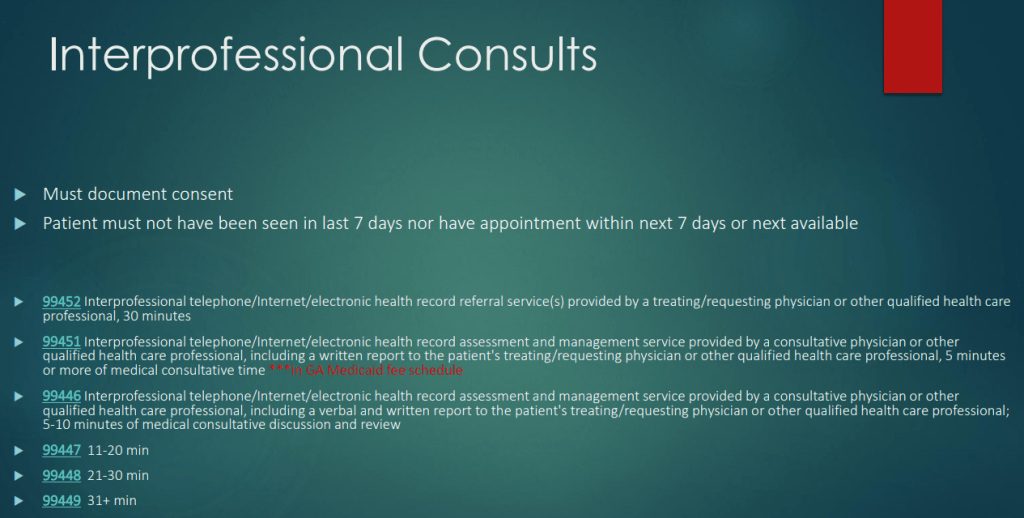
- 99451 –>interprofessional consultation (if patient consented). If an ED physician calls for consultation, documentation could allow for this code as long as the patient is not seen before or after within 7 days
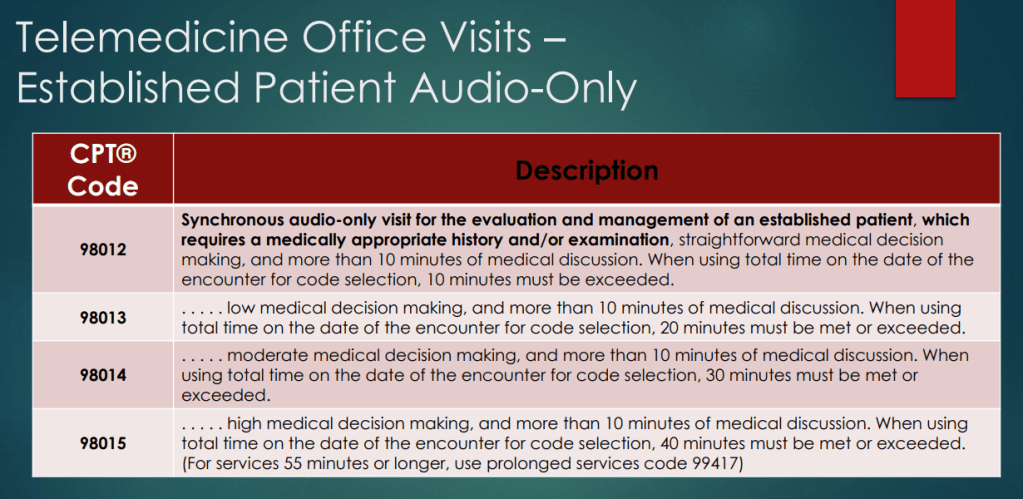
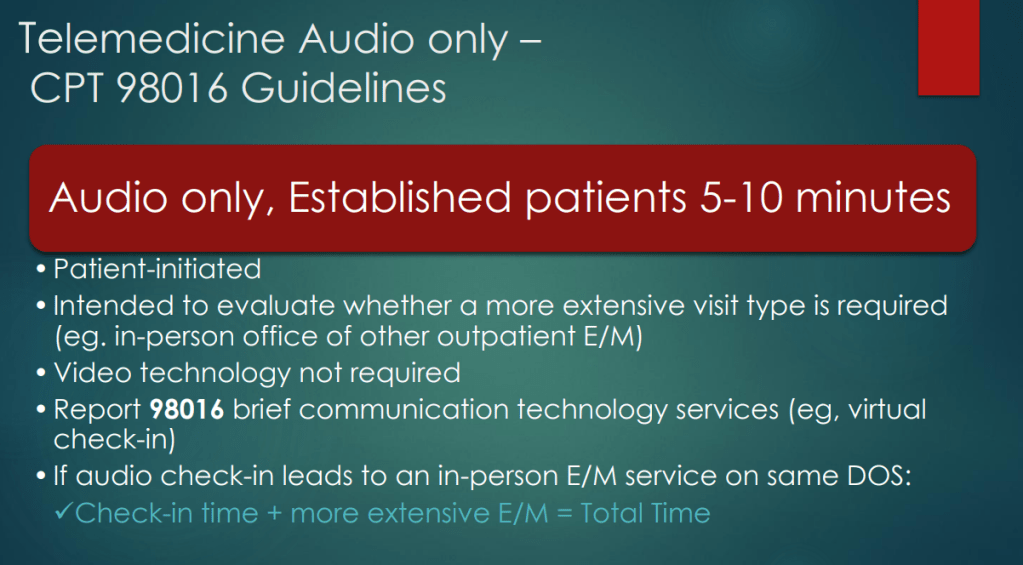
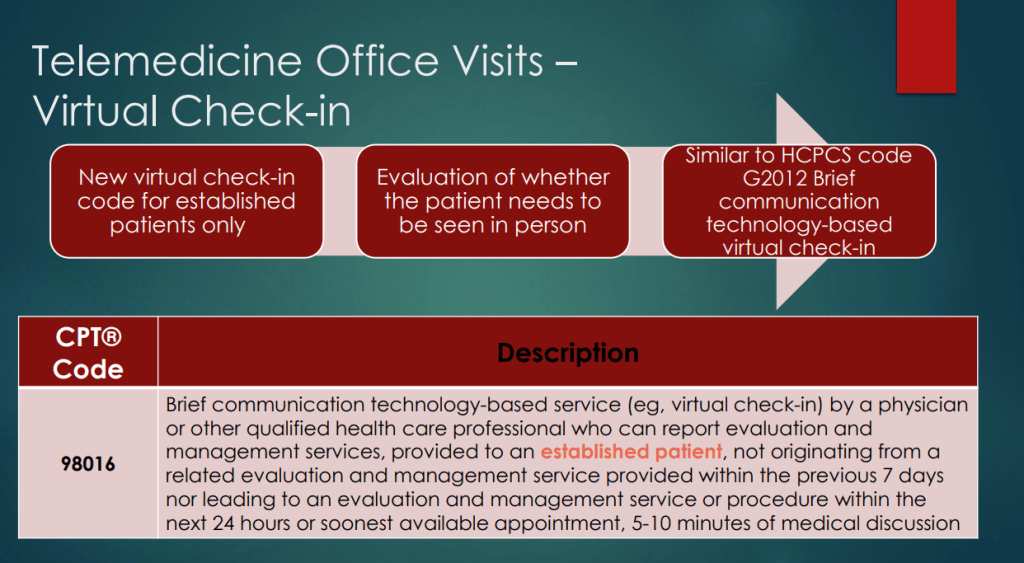
- 98016 –>audio (telephone) consult code for established patients. This could be used to check in to see if the patient needs an office visit
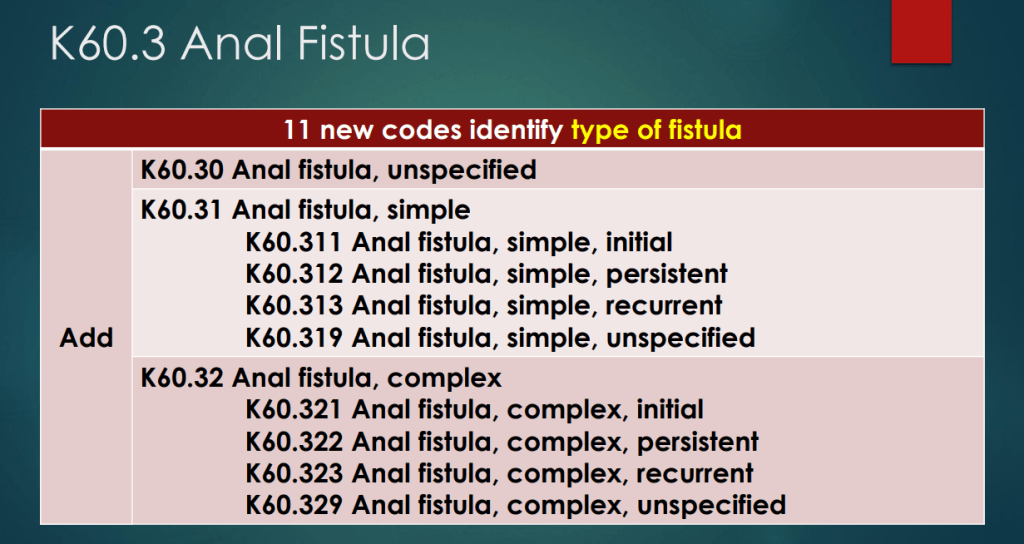
- New ICD-10 codes for IBD with fistulas, BMI codes and eating disorders


- If a patient is seen in ED and leaves ED, recommended to use ED codes, not office-based outpatient codes
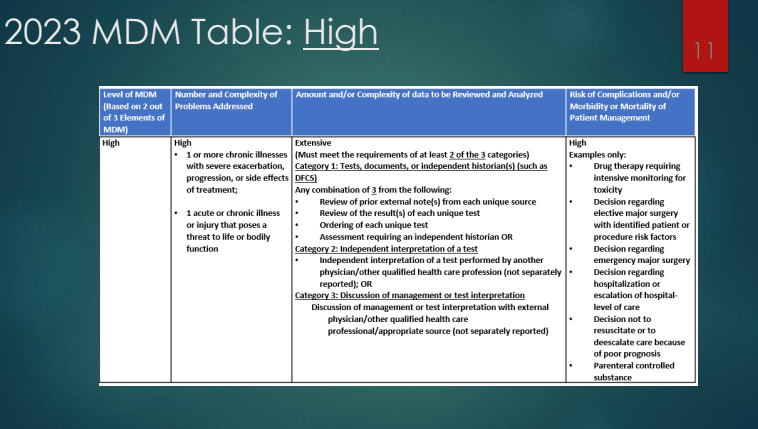
- For inpatients, HAL management is generally a high risk medication/treatment for coding-billing purposes
- Document defensively. Increasingly, insurance companies are trying to downcode visits. Recommend resisting this and document why the initial codes were selected
- Except for Medicaid, can use modifier 25 and bill if patient seen in clinic by one provider and in the hospital by another provider, if each was involved in patient care