- Z Li et al. Liver Transplantation 2025; 31: 1337-1348. Living-donor availability improves pediatric patient survival in a large North American center: An intention-to-treat analysis
- AG Feldman, MA Adams. Liver Transplantation 2025; 31: 1318-1319. (Editorial) Open Access! Living donor liver transplant offers pretransplant and posttransplant pediatric survival advantages
“A rising tide lifts all boats” has been used to express the sentiment that a good economy is beneficial to all. However, this has been criticized as not all boats are lifted equally and some boats are a lot nicer than others. I was thinking about this expression with these recent publications. The articles indicate that the availability of living donor liver transplant (LDLT) is clearly beneficial to the recipients but also is helpful, in a lesser way, to others on the transplant list as well.
Researchers analyzed data from 474 pediatric candidates listed for liver transplants at a single center from 2001 to 2023 (Toronto).
Key findings:
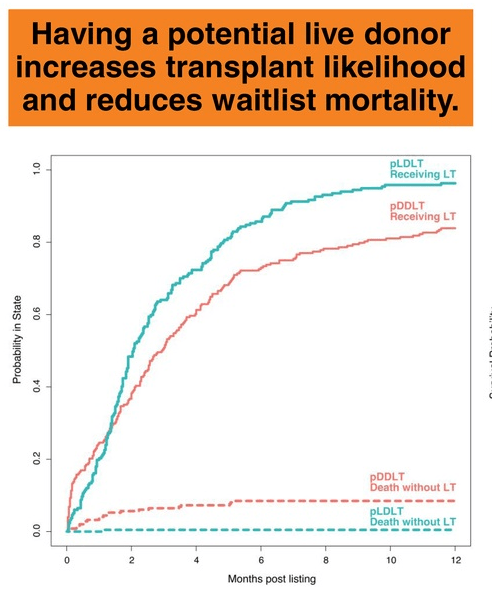
- The pLDLT group had a higher likelihood of receiving a liver transplantation (adjusted HR: 1.38) a lower risk of dying without a transplant (adjusted HR: 0.11)
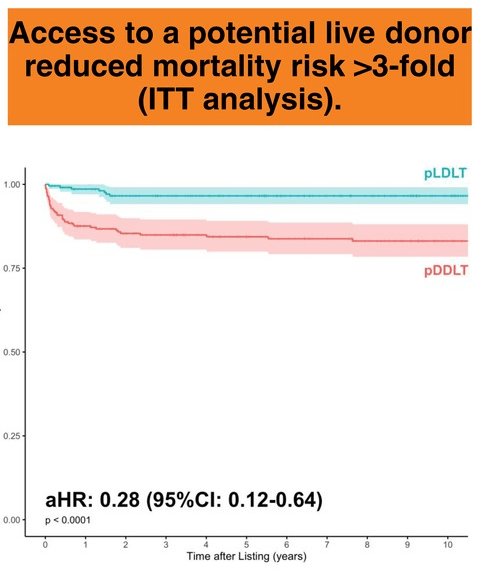
- Survival rates from the time of listing were significantly better in the pLDLT group compared to the pDDLT (on live donor) at 1—(98.6% vs. 87.6%), 5—(96.6% vs. 84.4%), and 10—(96.6% vs. 83.1%) years
- Having a potential live donor was linked to a 72% reduction in mortality risk (adjusted HR: 0.28)
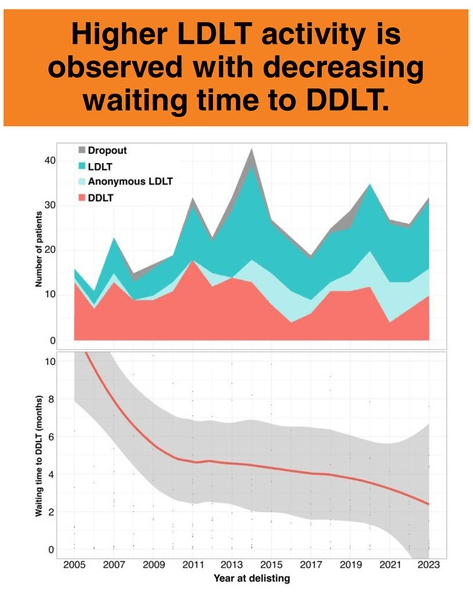
- The waiting time for deceased donation shortened. This correlated with increased LDLT utilization, suggesting LDLT not only improved outcomes but also shortened wait times even for pDDLT patients
From the associated editorial:
- “LDLT continues to be underutilized in the United States with only 15% of all pediatric LTs being LDLTs.1… In 2024, only 6 pediatric centers across the United States performed 5 or more LDLTs.6…”
- “Black and African-American and Hispanic candidates and those with public insurance are half as likely to undergo LDLT compared with Caucasian candidates and those with private insurance.7,8“
- “In a survey of over 200 parents of pediatric candidates and recipients of LT, only 72% reported knowing the steps to gain access to LDLT, and only 69% knew that donor costs were covered by the recipient’s insurance.7“
- The authors recommend collaboration between centers offering LDLT and those that don’t so that more patients could benefit
My take: More use of LDLT will result in better outcomes.
Related blog posts:
- PRO and CON: All Pediatric Transplant Centers Should Have Living Donor Liver Transplant Option
- What Can Go Wrong with Living Liver Transplantation for the Donor
- How to Improve the Gift of Life
- How to Lower Pediatric Liver Transplantation Waitlist Mortality
- Liver Transplant Outcomes in Children: Two Studies
- Anonymous Nondirected Liver Donors
- More on Time to Split (2018)
- What is Driving Racial Disparities in Access to Living Donor Liver Transplants
