Case history: A well-nourished previously healthy 20 month old was admitted to the hospital with a one week history of frequent vomiting. He had a history of frequent lint ingestion. He had been seen by three different health care providers during the week prior to his admission.
At the time of admission, he had numerous electrolyte derangements (Na 124, K 3.2, CL 76) and acute kidney dysfunction with a BUN of 118 and Creatinine of 3.06. He had severe multisystem disease including severe ventricular dysfunction (BNP 2196). He needed an oscillator ventilator, dialysis and cardiac medications (including epinephrine, and milrinone).
He had an extensive evaluation. After he had stabilized and then markedly improved (12 days after admission), an UGI study demonstrated an obstruction near the 2nd-3rd portion of the duodenum with a dilated proximal duodenum.
UGI study:

Due to the obstruction which was thought to be anatomic, the GI service deferred management to pediatric surgery. The surgical service requested GI inspection with endoscopy immediately prior to surgery. If a bezoar was identified, the surgical plan was for a mini-laparotomy. If not, the surgical plan was for laparoscopy repair.
Endoscopy findings: There was a narrowed opening (different orientation of same narrowing in both pictures) with a string-like material.

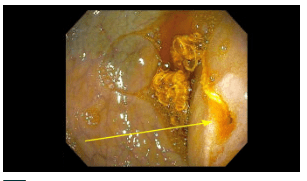
Surgical findings: A duodenal web with a piece of lint was identified. The patient had a laparoscopic wedge excision with a transverse closure of the duodenotomy. The lint may have occluded the tiny opening of the web that he had been living with since he was born.
My take: This is the first time I have seen the endoscopic appearance of a duodenal web.
In my view, this was a ‘great case.’ In a commentary by Jerome Groopman (N Engl J Med 2004; 351:2043-2045), his wife noted that a case is “a great case because you not only make the diagnosis — you do something fundamental about it. You can really help.” However, Dr. Groopman stopped using the words, ‘a great case’ after his personal experience when his son was severely ill as an infant with a bowel obstruction due to intussusception: “For me and for Pam, the experience had no resonance of “a great case.” There was no intellectual pleasure in solving a clinical puzzle, no charge of exhilaration from the drama of the operation. Instead, there was terror, raw and palpable, as we realized how close we had come to burying our first son….I still find myself unable, except in retrospect, to retrieve the language of my youth and speak about “a great case.” It is as if medicine at this stage of my life has split into two streams — a current of marvelous biology and an undertow that pulls at the soul.”
