J Sabella et al. JPGN 2023; 76: 282-287. Multidisciplinary Tiered Care Is Effective for Children and Adolescents With Rumination Syndrome
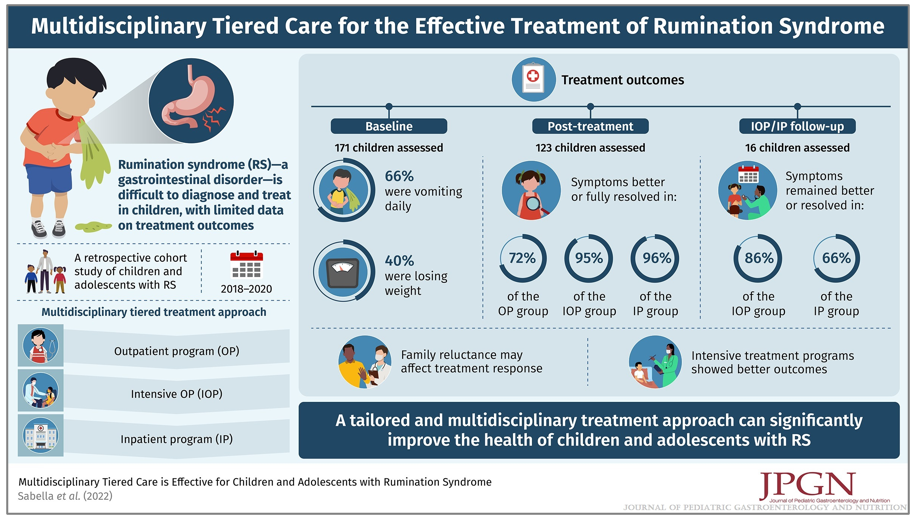
The was a retrospective single-center study (n=171). The median length of treatment was 6.5 months for outpatient care, four days for intensive outpatient care and nine days for intensive inpatient care.
Key findings:
- After treatment, 72% of OP, 95% of IOP, and 96% of IP patients reported that symptoms were better or fully resolved compared to baseline
- In a subset of 16 children, At follow-up (median 5.3 months), 86% of IOP and 66% of IP patients had symptoms that remained better or resolved.
- The authors found “an association between patient or family reluctance to accept the diagnosis of rumination syndrome and a lack of response to treatment. Prior studies have demonstrated the importance of commitment and belief in the process of treatment and/or fully commit to the behavioral treatment process as a barrier to care.”
In a commentary on this article from Pediatrics Nationwide, Dr. Peter Lu noted: “What was striking to me was how effective the intensive treatment programs are. Both of those groups included the most severe of patients, oftentimes, they’ll have a feeding tube or a central line for parenteral nutrition. Even in that selected, very severe refractory group, we had very good response rates to treatment…RS is a disorder that cannot be effectively treated by a GI doctor alone…Treatment of RS involves a GI doctor and a GI psychologist, and we oftentimes will involve one of our GI dieticians”
My take: This study shows that treatment can be very effective in treating rumination syndrome, especially if the patient/family is amenable to therapy.
Related blog posts:
- The Half Empty Glass: Rumination Outcomes
- Internet Survey: Lots of People Have Rumination
- Expert Advice for Diagnosis and Treatment of Rumination Syndrome
- Baclofen for Rumination
- Dupixent for Eosinophilic Esophagitis (1-11 yrs) and Clinical Diagnosis of Rumination from DDW Tweets
Also, good tips on managing rumination were given on a bowel sounds podcast: Desale Yacob & Ashley Kroon Van Diest – Rumination Syndrome (August 2021)