JL Yasuda et al. J Am Coll Surg 2024; 238: 831-843. Surveillance Endoscopy in Pediatric Esophageal Atresia: Toward an Evidence-Based Algorithm
This retrospective study examined 546 children with esophageal atresia (EA) who underwent 1,473 surveillance endoscopies (2004-2023). The authors defined a hiatal hernia as at least 1 cm of gastric folds present above the level of the diaphragmatic pinch. “Actionable findings” were any finding that prompted a change in management.
Key findings:
- A total of 770 endoscopies (52.2%) in 394 unique patients (72.2%) had actionable pathology
- The most common actionable finding was esophagitis which lead to escalation of therapy (484 endoscopies in 32.9% of patients). However, de-escalation of therapy was common as well; this occurred in 233 patients (after 310 endoscopies)
- Barrett’s esophagus (intestinal metaplasia) was identified in 7 unique patients (1.3%) at a median age of 11.3 years. 6 of 7 patients with Barrett’s were receiving acid suppression at time of diagnosis
- Actionable findings leading to surgical intervention were found in 55 children (30 refractory reflux and 25 tracheoesophageal fistulas).
- Significant predictors of actionable pathology included increasing age, long gap atresia, and hiatal hernia.
- Symptoms were not predictive of actionable findings, except dysphagia (OR 5.80), which was associated with stricture.
- Acid suppression was associated with a reduced odds of actionable findings (OR 0.78); however, there was still a high rate of actionable findings in this group. 51% of endoscopies while a patient had been receiving acid suppression had actionable findings.
- Fundoplication was NOT associated with protection against actionable findings (OR 1.42)
- Table 2 notes that 52 (3.5%) patients had eosinophilic esophagitis therapy escalated. Infrequently, non-esophageal diseases were identified: Celiac in 3 patients (0.2%), Crohn’s disease in 2 patients (0.1%), eosinophilic gastritis and/or duodenitis in 2 (0.1%), and H pylori in 4 patients (0.3%).
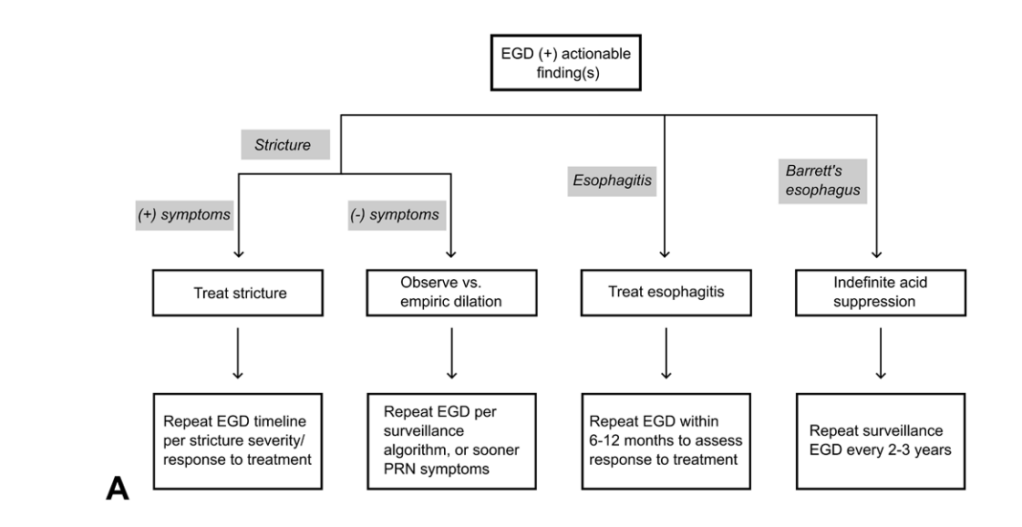
Proposed Management Algorithms:

Discussion Points (from authors):
Take multiple levels of esophageal biopsies: “Any surveillance esophagogastroduodenoscopy (EGD) should at minimum include 2 to 3 levels of esophageal biopsies”
Acid suppression recommendations: “Barrett’s esophagus is proposed to be an absolute contraindication to acid suppression wean; relative contraindications to weaning acid suppression include earlier erosive esophagitis, earlier failed acid suppression discontinuation attempt(s) with rebound esophagitis, or hiatal hernia; if acid suppression is weaned in these high-risk situations, we believe close follow-up endoscopy is warranted to assess for rebound pathology [which happened in nearly 20%].” And, “our practice is to empirically de-escalate acid suppression in children without contraindications to doing so when there is no gross esophagitis and biopsies show no or minimal inflammation (generally less than 5 eosinophils per high powered field).”
Consider doing endoscopy off acid suppression for approximately three months: “To maximize the information yield from the initial endoscopy, a patient may first wean off acid suppression approximately 3 months before endoscopy to permit evaluation for both anatomy and esophagitis off acid suppression. Subsequent surveillance is performed
according to our algorithm and within at most 6 to 12 months of any acid suppression changes.”
The authors do not generally recommend pH-Impedance. “There are no consensus “normal” values for pH-impedance reflux parameters in either healthy or EA children, and pH-impedance has failed to show any predictive correlation with actual esophagitis in multiple pediatric studies. In particular, children with EA with “normal” numbers of reflux events cannot adequately clear their refluxate in the context of poor esophageal motility and can still develop reflux injury. pH-impedance tracings in EA require manual review by an experienced reader, with automated analysis being highly unreliable in the setting of low baseline impedance values.”
Limitations: 1. Some of the actionable findings may have been expected based on prior endoscopies (e.g. prior stricture) and could influence value of symptoms like dysphagia. 2. This population was skewed to patients with more severe EA as it is a subspecialty center. One indicator was that their group had 24% with long-gap EA compared to an overall expected rate of 10% in the general EA population 3. Retrospective study 4. Many of the patients were not truly “surveillance” endoscopies but were done due to reported symptoms
My take: It’s unfortunate that this article did not get published in a more mainstream pediatric journal (e.g. JPGN, J Pediatr, Pediatrics) or a more mainstream gastroenterology journal (eg. Gastroenterol, Clin Gastroenterol Hepatol, AJG) as this article provides a lot of great data and useful advice. More than 70% of subjects had actionable findings during the course of their follow-up, including more than 40% of 1 year-olds.
The algorithms above suggest that at minimum, EA patients should have endoscopy every 5 years (likely starting between 12-18 months). More frequent endoscopy (every 2-3 years) may be worthwhile in those with risk factors (e.g. long gap EA, hiatal hernia, and prior esophagitis) and follow-up endoscopy is needed sooner if change in therapy (stricture dilation, esophagitis treatment or treatment de-escalation).
Related blog posts:
- Guidelines for esophageal atresia-TEF
- Endoscopic Surveillance after Esophageal Atresia: Low Yield in Pediatrics This study wit 209 patients (Koivusalo et al. JPGN 2016; 62: 562-66) reported that “routine endoscopic surveillance had limited benefit and seems unnecessary” before 15 years of age.
- Do PPIs Increase the Risk of Eosinophilic Esophagitis in Patients with Esophageal Atresia?
- How Long Should Be PPIs Be Used in Patients with Esophageal Atresia?
- How Effective are Stents for Anastomotic Esophageal Strictures in Patients with Esophageal Atresia
- More Often Than Not Esophagitis in Children with Esophageal Atresia is NOT due to Reflux
- Esophageal Diseases Special ~15% of Healthy Individuals have microscopic esophagitis
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.
