A Anafy et al. JPGN 2024; 79:325–334. Acute pancreatitis in children with inflammatory bowel disease: Risk factors, clinical course, and prognosis
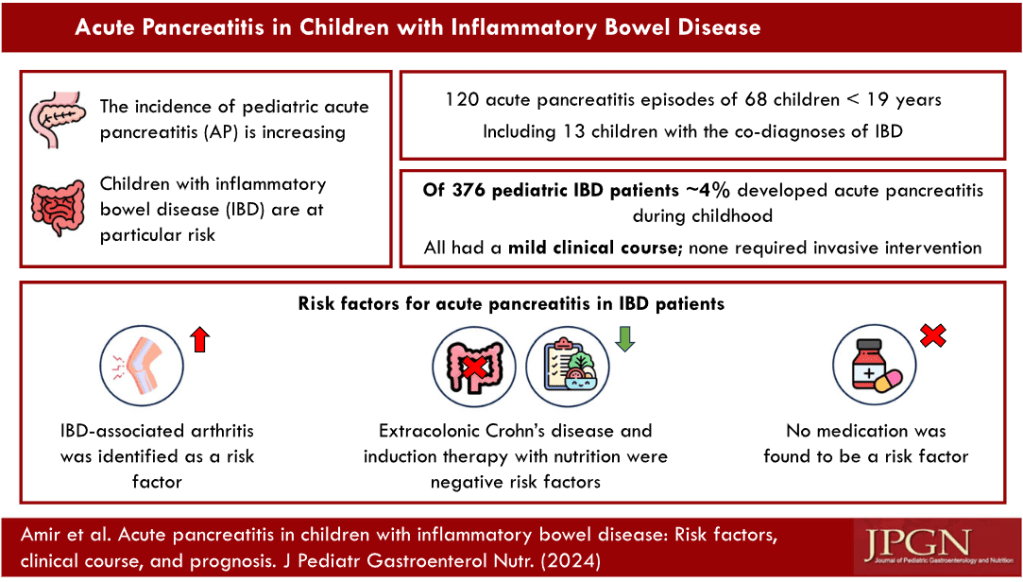
In this retrospective study with 376 children, Key Findings:
- 4% of patients with pediatric IBD developed acute pancreatitis (AP)
- The presumed etiology for AP in all IBD patients was IBD-related: IBD flare-up in five, side effects of medications in two, and undetermined in seven.
- The only risk factor for AP development among IBD patients was IBD‐associated arthritis (23% vs. 3% for IBD‐non‐AP).
- Extracolonic Crohn’s disease emerged as a negative risk factor for AP: it was present in only 2/13 (15%) IBD‐AP patients compared to 20/39 (51%) IBD‐non‐AP patients (p = 0.05). Patients who receive induction therapy with nutrition (exclusive enteral nutrition or Crohn’s disease exclusion diet) were less likely to be present in the IBD‐AP group (1/12 [8%] vs. 17/39 [44%] IBD non-AP patients, p = 0.04.
- This study population, at the time of AP, had a relatively high number treated with ASA agents (66%; 11/14 AP-IBD and 26/42 Non-AP-IBD)), 27% with azathioprine (6/14 with AP-IBD and 9/42 Non-AP-IBD), and low number receiving biologics (18%, 2 AP-IBD and 8/42 Non-AP-IBD
My take: This study shows that acute pancreatitis is common in children with inflammatory bowel disease.