I Hanna-Jairala, DA Drossman AJG 2024; DOI: 10.14309/ajg.0000000000002800. Open Access! Central Neuromodulators in Irritable Bowel Syndrome: Why, How, and When
This is a terrific review article. The authors detail the rationale for neuromodulators, strategies for selecting among them, side effects, and dosing.
Background: “IBS is frequently associated with neuropsychiatric disorders such as depression and anxiety, which are considered triggers for the onset of symptoms or occur in response to having them (3). In the Rome Foundation global study that included 54,127 participants, subjects with psychological distress or clinically relevant somatic symptoms were 4.45 times more likely to have 1 or more DGBI than those without psychological distress. The same study reported that those who met specific criteria for bowel disorders presented clinically relevant psychological distress or somatic symptoms in 55.5% of cases (4). In addition, in a meta-analysis that included 7,095 subjects with IBS exclusively, the global prevalence of depression was 36%…Anxiety was present in 44% of patients with IBS….Central neuromodulators act on receptors along the brain-gut axis, so they are useful in treating psychiatric comorbidities, modifying gut motility, improving central downregulation of visceral signals, and enhancing neurogenesis in patients with IBS… Neuromodulator treatment is still considered off-label, many of the recommendations herein are based on expert consensus (6)”
Key points:
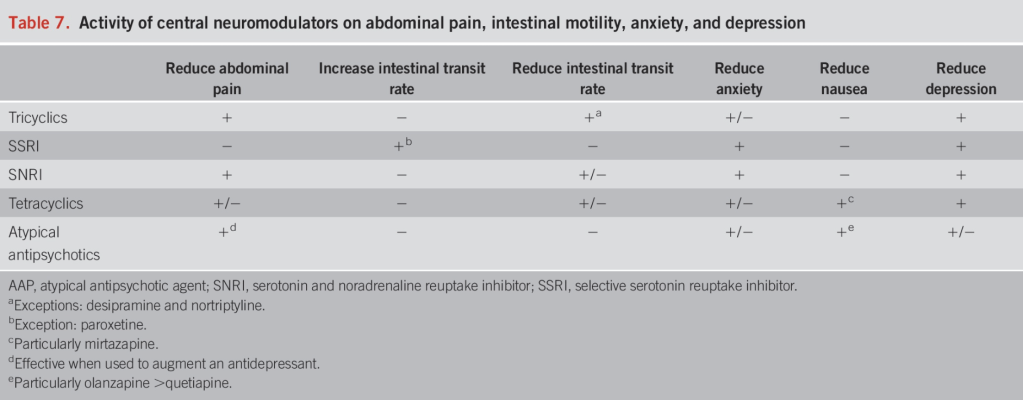
- “The first-line treatment for pain management in IBS is using tricyclic antidepressants.” Nortriptyline and desipramine are less likely to cause constipation.
- “Selective serotonin reuptake inhibitors (SSRIs) are useful when symptoms of anxiety and hypervigilance are dominant but are not helpful for treating abdominal pain….The SSRIs include fluoxetine, fluvoxamine, sertraline, paroxetine, citalopram, and escitalopram. …Sertraline, citalopram, and escitalopram tend to have the fewest pharmacokinetic drug interactions”
- “SSRIs are first-line pharmacologic agents for treating anxiety disorders, but they have the potential to induce restlessness and exacerbate anxiety when the drug is initiated. They are typically initiated at half of the usual starting dose to minimize these potential anxiogenic adverse effects. The dose may gradually increase to the regular starting dose after about 1 week… SSRIs should be considered when a significant component of anxiety without pain is present.”
- SNRIs: “In addition to showing benefits with depression and painful disorders, SNRIs have shown significant improvement in anxiety.” Thus, they may be useful as monotherapy for patients with pain and anxiety.
- Tetracyclics: “The most representative agent of this class is nirtazapine (Table 5). However, their effects seem to be mainly on anxiety, early satiety, nausea, and other symptoms associated with esophageal and gastroduodenal disorders, so their use in IBS is limited.”
- “It is important to explain to the patients, …neuromodulators are not necessarily used for the treatment of depression but are a therapeutic alternative in the management of DGBI. It helps to use the term “neuromodulator” instead of “antidepressant” (6,8) It also helps to clarify that these medications can treat pain and other GI symptoms independent of treating depression, and the dosages are often lower than those used for treating major depression. This will preclude any patient concerns that their symptoms are being underestimated or considered to be in their head (6,8).”
- Using central neuromodulators for IBS requires long-term treatment. From our experience, 6–12 months of treatment or more are needed to increase the likelihood of remission.
Related blog posts:
- Educating Families About Chronic Pain (2024). This is a very helpful article explaining how to educate families about chronic pain
- “How to Approach a Patient with Difficult-to-Treat IBS”
- Atlantis Study: Possibly Best Evidence That Tricyclics May Help Irritable Bowel
- Electrocardiograms -Will We Ever Know If They Are Useful Prior to Tricyclic Antidepressants?
- Jose Garza: What’s New in Motility (Part 2)
- It Hurts Here and Here and Here
- Brave New World: Psychotropic Manipulation & Pediatric Functional GI Disorders (2014)
- A (Virtual) Reality Without Pain?
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.

Would be great to see more discussion on CBT and hypnotherapy. Even a comparison to neuromodulator use. The American take on healthcare, give it a pill! Some of these treatments take months to see impact, putting that same amount of time into a non-drug treatment may be more beneficial in the long run.
Agree that non-pharmacologic options need to be used more. That said, it is often difficult for families to find qualified providers in a timely & cost-effective manner.