We had a great pancreas update lecture from Dr. Jay Freeman. In my view, a great lecture involves a well-delivered informative lecture that likely leads to an improvement in clinical practice. My notes below may contain errors in transcription and in omission. Along with my notes, I have included many of his slides.

- About 10% of patients with acute pancreatitis already have damage indicating chronicity
- Severe pancreatitis is often defined by degree of organ dysfunction (eg. cardiac, pulmonary, renal). A practical definition of severe pancreatitis in children is whether the patient requires admission to an ICU

- The term “position paper” is typically used instead of “guidelines” due to lack of definitive data and reliance on expert opinion

- While the guidelines suggest 1.5-2.0 x maintenance fluid volumes, the benefit of this additional IVFs is not clear. Dr. Freeman’s clinical practice is often to start with 1.5 x maintenance rate and to try to transition to enteral diet

- Aggressive fluid resuscitation of acute pancreatitis in adults is associated with increased risk of fluid overload. Lactated ringer’s is generally fluid of choice.
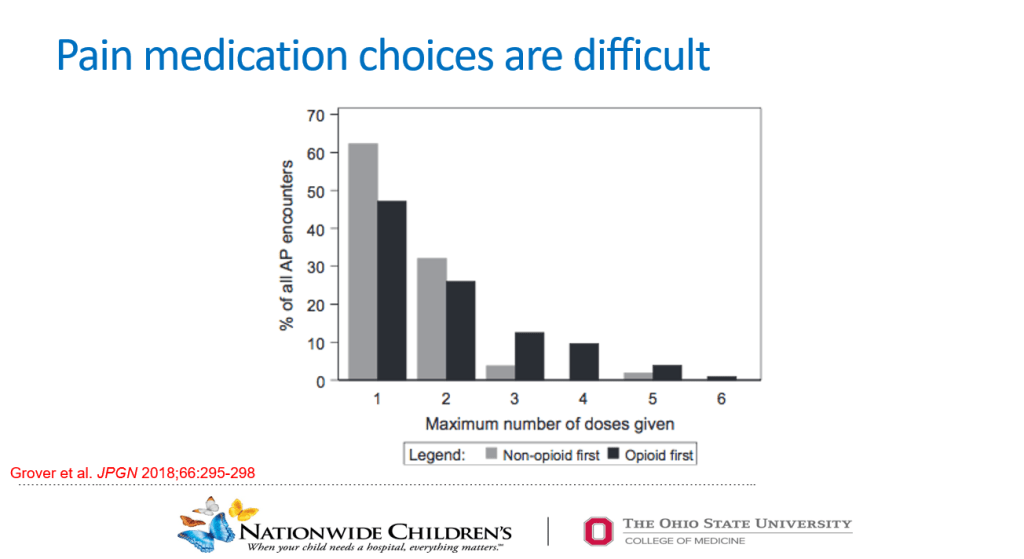
- In this study with 211 pediatric patients, starting with a narcotic increases the likelihood of continuing with narcotics. Many patients can respond to acetaminophen and NSAIDs. Using narcotics, may increase the risk of sensitization to pain (lowering pain threshold)

- In this study with adults (Not Randomized), use of PCA was associated with longer hospitalizations, slower start to enteral nutrition and increased narcotic use at discharge

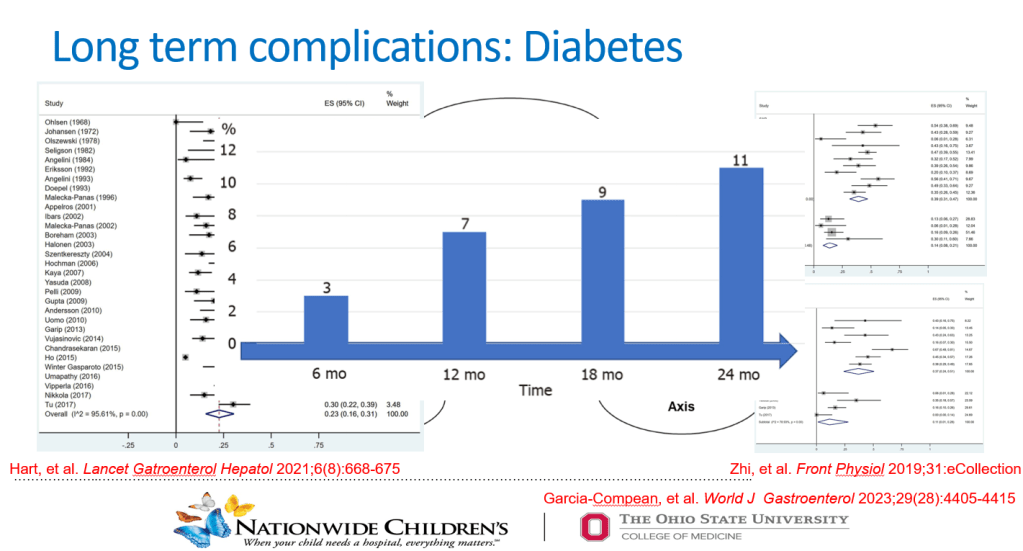
- A single episode of acute pancreatitis, even mild cases, is associated with long-term risks including risk of exocrine pancreatic insufficiency (often transient), increased risk of diabetes mellitus and even pancreatic cancer.
- Restricting fat in the diet for 1-2 weeks after an episode may reduce some symptoms
- Because of risk of complications, Dr. Freeman recommends follow up after hospitalization (after a few months) and for up to 5 years (at least for 2 years)
- Dr. Freeman indicated that he recommends checking genetic tests for pancreatitis if a patient has had more than one episode. If a patient is less than 5 years of age or has a significant family history, checking for genetic predisposition should be considered with the first bout of pancreatitis.
Key points: Even patients with acute pancreatitis need follow-up. Consider using non-narcotic medicines as the first line, especially in patients who have not ‘failed’ these medications.
Related blog posts:
- Medical Management of Chronic Pancreatitis in Children
- Acute Pancreatitis in Children with Inflammatory Bowel Disease
- NASPGAN Paper: Surgery for Chronic Pancreatitis: Choose Your Operation and Surgeon Carefully
- More Data Supporting Lactated Ringers for Acute Pancreatitis
- Imaging Recommendations for Pediatric Pancreatitis
- Diabetes Mellitus Associated with Acute Recurrent and Chronic Pancreatitis
- How Good Are Our Tests for Acute Pancreatitis?
- Choledochal Cyst and Pancreatitis
- Pediatric Pancreatitis -Working Group Nutritional Recommendations
- Consensus Pancreatitis Recommendations
- Acute Pancreatitis: NASPGHAN Clinical Report.
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.
