ZM Sellers et al. J Pediatr 2025; 276: 114298. Impact of Elevated Serum Triglycerides on Children with Acute Recurrent or Chronic Pancreatitis from INSPPIRE-2
Using the INSPPIRE-2 cohort of children with acute recurrent or chronic pancreatitis (CP) (n = 559), the authors compared the outcomes for children based on their triglyceride levels. Definitions: normal triglycerides (<150 mg/dL), any high triglycerides (HTG) (≥150 mg/dL, mild-moderate HTG (150-499 mg/dL), moderate HTG (500-999 mg/dL), and severe HTG groups (≥1000 mg/dL).
- Key findings:
HTG was not associated with an increase in the number of pancreatitis attacks per person-years - HTG was not associated with an increase in CP prevalence
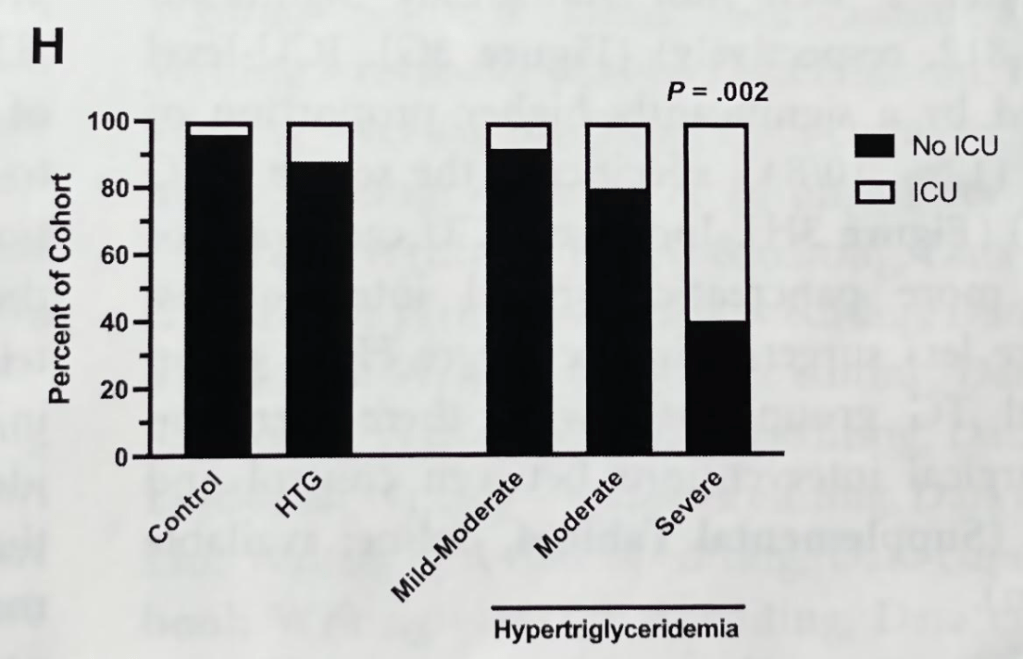
- HTG severity was associated with increased pancreatic inflammation, pancreatic cysts, pain, hospital days, number of hospitalizations, intensive care, and missed school days
- Interestingly, there were less pancreas gene variants in the severe HTG group which supports the notion that HTG can be a driver of pancreatitis disease
Discussion:
- “It is well-established that severe HTG levels increase pancreatitis risk by increasing serum chylomicrons and free fatty acids, causing pancreatic ischemia, acidosis and vascular injury…In adults, TG levels >/= 200 mg/dL are independently associated with pancreatic necrosis.”
My take: Checking triglyceride levels, which is in accordance with NASPGHAN recommendations, is a good idea. HTG is a potentially-modifiable risk factor for more severe disease. Levels that substantially increase the pancreatitis severity (500 or higher) merit treatment even in the absence of pancreatitis
Related blog posts:
