- L Godny et al. Gastroenterol 2025; 168: 952-964. Open Access! Mechanistic Implications of the Mediterranean Diet in Patients With Newly Diagnosed Crohn’s Disease: Multiomic Results From a Prospective Cohort
- MT Abreu et al. Gastroenterol 2025; 168: 872-874 (Editorial) Open Access! A Mediterranean Diet for Crohn’s Disease: Embracing Colorful Diversity to Improve the Microbiome
Methods: In this prospective cohort study, consecutive adults (n=271) from 2 large IBD centers in Israel with newly diagnosed CD were recruited and followed prospectively. MED adherence was assessed by repeated food frequency questionnaires (FFQs) using a predefined inflammatory bowel disease Mediterranean diet score (IBDMED score), alongside validated MED adherence screeners. Crohn’s disease activity index (CDAI), C-reactive protein, fecal calprotectin, and microbial composition (16S-ribosomal RNA sequencing) were assessed each visit. Baseline serum and fecal samples were analyzed for targeted quantitative metabolomics.
Demographic/Clinical data indicate 68% received biologics and 40% receiving immunomodulators. 32% received 5-ASA medications (despite lack of proven efficacy)
Key findings:
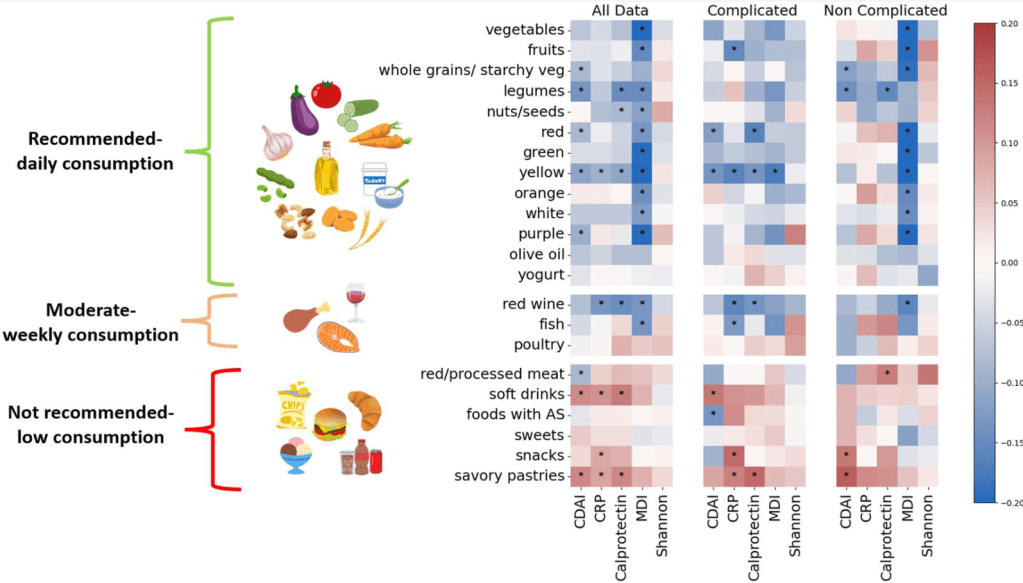
- Adherence to MED was associated with a noncomplicated CD course, and inversely correlated with CDAI, fecal calprotectin, C-reactive protein, and microbial dysbiosis index (all P < .05)
- Increasing adherence to MED over time correlated with reduced CDAI and inflammatory markers (P < .05)
- Adherence to MED correlated with a beneficial microbial cluster of commensals and short-chain fatty acid producers including Faecalibacterium, and with plant metabolites, vitamin derivatives, and amino acids
- Adherence to MED in the cohort group was comparable to the general non-IBD population in Israel
Limitations: This was an observational study rather than an interventional study with a control group. Thus, the results could be influenced by reverse causality
In the associated commentary by Abreu et al, it is noted that in Israel, “MED is more commonplace than in the US and other Western countries…Godny et al found that IBD patients had an average MED adherence score of 7.8, which is similar to that of the general non-IBD population in Israel; in contrast, the average MED adherence score in the US is 4–5.Godny et al’s CD patients consumed an average of 21 g of fiber per day; in a study we just completed, American CD patients consumed less than half that amount.13 Indeed, the baseline diets of American IBD patients are characterized by high amounts of saturated animal fat and almost no fresh fruits and vegetables…Another difference between the Israeli population and the typical American population is body mass index (BMI). The average BMI of patients in this study was 21.9 kg/m2 (interquartile range 20–25.3 kg/m2). This contrasts with the average BMI of the general US population of 30 kg/m2.”
My take: This study shows an association between MED diet and better outcomes/less complications in adults with Crohn’s disease. Eating a good diet is an important part of treatment.
Additional notes on dietary scores: “The IBDMED screener positively scored high consumption of MED-recommended dietary components such as fruits, vegetables, olive oil, legumes, nuts and seeds, and fish. It also positively scored low consumption of MED non-recommended dietary components such as red and processed meat, soft drinks, and sweets. To this we added several dietary features based on previous data associated with microbial composition and function. These included a positive score for plant diversity27 by scoring for different colors in the diet, consumption of fermented foods28 (specifically yogurt), and inclusion of starchy vegetables like potato in the whole grain category to promote diversity in the carbohydrate-rich food group, as well as support butyrate producers as we had previously shown.29 In addition, we aimed to positively score for relatively low UPF intake. To this end, we evaluated the average intake of sweets, snacks, sweet and savory pastries, soft drinks, and foods and drinks containing artificial sweeteners.”
Related blog posts:
- Mediterranean Diet vs Specific Carbohydrate Diet for Crohn’s Disease
- AGA Guidance: Nutritional Therapies for Inflammatory Bowel Disease
- Trial by Diet Approach for Crohn’s disease in children (this blog post has link to 16 other dietary therapy posts)
- The Quality of Evidence for Dietary Treatments in Inflammatory Bowel Disease
- Dr. Maria Oliva-Hemker: Positioning Therapies for Pediatric Crohn’s Disease
- Trial by Diet Approach for Crohn’s Disease in Children
- More Evidence That A Proinflammatory Diet May Increase the Risk of Crohn’s Disease
- Pushing the Boundaries on Dietary Therapy for Crohn’s Disease (CD-TREAT)
Also, from Kim Beall, Cofounder and Managing Director of Nutritional Therapy for IBD:
“If you haven’t been to the website recently, we have expanded the recipe database to over 1,000 recipes with many filterable aspects and we’ve just released a new nutrition tool, the IBD Nutrition Navigator to facilitate nutrition conversations between providers and patients to find the right nutritional starting point. This is a project led by Dr. Ananthakrishnan and a dedicated team of pediatric and adult medical advisors in a two year long development process. Many have told us this is a useful tool particularly for those less familiar with nutrition in IBD. We’re excited about it’s potential to integrate nutrition in practice, with “an option for every patient”. We appreciate your support in sharing our information, tools, and resources to advance IBD nutrition care.” Here’s the link to their website:
