A Turunen et al. JPGN Reports. 2025;6:312–315. Elevated tissue transglutaminase immunoglobulin A: Celiac disease or polytypic plasmacytosis?
Briefly noted: The authors present a case report of an adolescent girl post cardiac transplant with hypergammaglobulinemia and presumed celiac disease (CD), who had a persistently elevated anti‐tissue transglutaminase immunoglobulin A despite a gluten free diet. Ultimately, she was diagnosed with polytypic plasmacytosis from suspected immune dysregulation.
Key point:
- This case serves as a reminder that when treating those with persistently elevated tTG IgA on a strict GFD, etiologies outside of CD need to be considered.
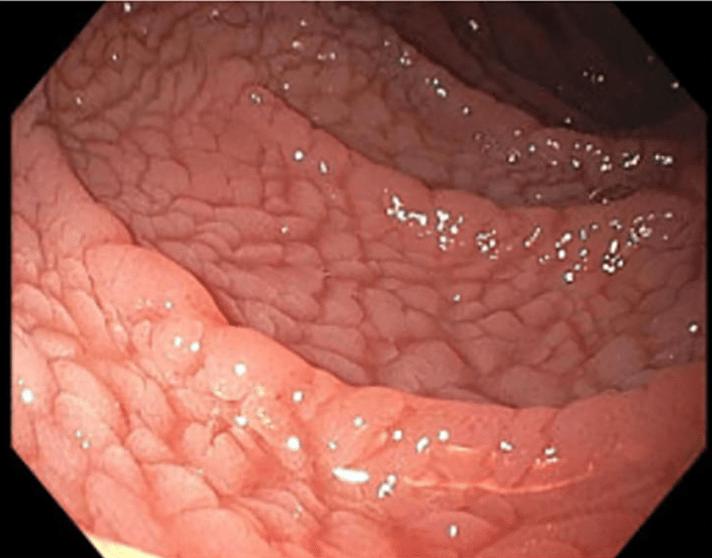
My take: I had a young girl several years ago who had celiac diagnosis at an outside institution. She had multiple autoimmune disorders. After not responding to treatment, she had a follow-up panendoscopy showing ongoing IELs in duodenum and villous blunting. These findings were noted in the ileum as well. On reviewing her initial biopsies, the pathologist indicated that her findings could be celiac but it was suspected to be an immune dysregulation. Subsequently, she was diagnosed with CTLA4 deficiency and had a marked response to abatacept therapy.
Related blog posts:
- Immune Dysregulation and Inflammatory Bowel Disease
- Shorts: Hep E in Urine, Genetics in Autoimmune Enteropathy, EndoFlip Findings in EoE
- Targeted Therapy for Autoinflammatory Very Early Onset Inflammatory Bowel Disease
- Double Whammy: Coexistent IBD and Celiac Disease in Children
- Seronegative Villous Atrophy
- @AmyOxentenkoMD: Celiac Disease and Mimics
- Dr. Arun Singh: Tips and Tricks to Managing Celiac Disease
- Celiac Disease: Pro Tips (Part 4)
- 2023 ACG Celiac Guidelines for Adult and Children
- Lessons in Diarrhea (part 1)
- Patterns and Puzzles with Very Early Onset Inflammatory Bowel Disease
- VEO-IBD -Useful “Position” Paper is Really a Review
