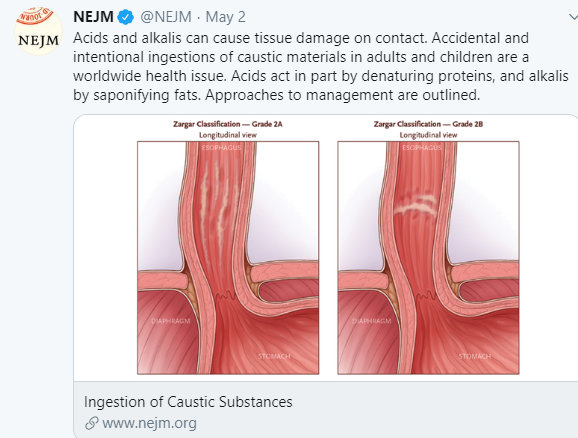
P Quitadamo et al. J Pediatr Gastroenterol Nutr. 2025;81:11–17. The effects of liquid bleach ingestion on children’s esophageal and gastric mucosa
Background: It has been recently reported that household bleach ingestion cause no or low-grade esophagitis in adults.13
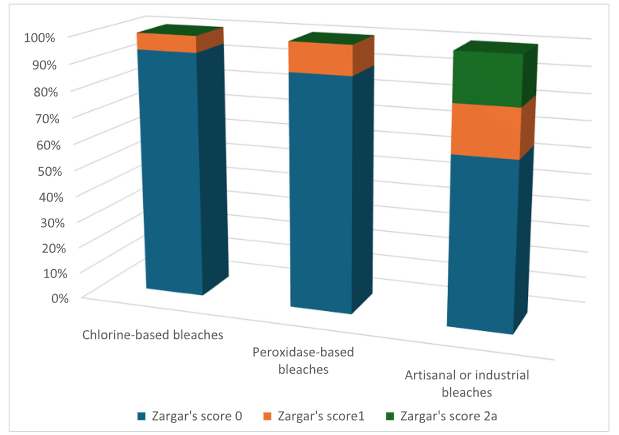
Methods: This prospective observational study was carried out between January 2017 and December 2023. One hundred children with a mean age of 58.7 months were included and divide into three groups. Group 1, children who had ingested household chlorine-based bleach; Group 2, children who had ingested household peroxidase-based bleach; Group 3, children who had ingested artisanal or industrial bleaches.

Key findings:
- Eighty-nine/100 (89%) children had ingested household bleaches (both chlorine- or peroxidase-based) while 11/100 (11%) had ingested homemade or industrial bleaches
- 73/100 (73%) patients were symptomatic. The most commonly reported symptoms were vomiting and drooling
- 13/100 (13%) were intentional with self-injurious or suicidal purposes
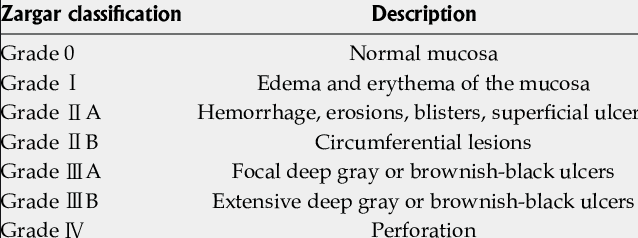
- Among the 71 children who performed EGD, no children reported severe esophageal lesions
- Zargar’s score 2a in 2/71 (2.8%). Both patients who reported moderate esophageal mucosal lesions (Zargar’s grade 2a) had ingested a homemade NaOCl-based (sodium hypochlorite) bleach with unknown dilution
- Gastric injury was reported in 6/71 (8.5%) patients, including hemorrhagic gastritis in one child. Among these children, five had ingested an artisanal or industrial bleach, and two had ingested a peroxidase-based bleach
My take (borrowed from authors): “Endoscopy is generally unnecessary in case of household bleach ingestion …[but] should be performed in children who ingest homemade or industrial bleaches.” Children having ingested commercially available household bleaches did not report significant mucosal lesions. The authors also advocated endoscopy in those with large volume ingestions (>100 mL) if symptomatic.
Related blog posts:
- Why Ingestion of Caustic Substances is Not A Good Idea The authors advocate a selective approach towards endoscopy in young children. “For children with only vomiting or drooling and those who refuse to drink, overnight observation is routine, and endoscopy is performed only if symptoms persist and the child remains unable to take oral fluids” If there is vomiting and drooling or stridor alone, endoscopy is recommended.
- Early Management of Caustic Ingestions in Children
- Detergent Pod Ingestions -Is an Endoscopy Needed? | gutsandgrowth
- New caustic danger from detergent pods
- Great website for families: www.upandaway.org
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition