This blog entry has abbreviated/summarized the presentations. Though not intentional, some important material is likely to have been omitted; in addition, transcription errors are possible as well. Link to full syllabus:
PG Course Syllabus 2014
The Dreaded Wake-Up Call (Part A) –Maercedes Martinez (NY Presbyterian Hospital) (pg 55 syllabus)
Variceal Bleeding – “When RED is not attractive”
Discussed presentation of varices (gastric/esophageal), etiologies, association with portal hypertension. Reviewed variceal grading.
Medical management:
- PICU admit
- Avoid over-transfuse (goal ~ 8 g/dL)
- Correct coagulopathy
- Role of platelets is controversial/if trouble with endoscopy, may be helpful
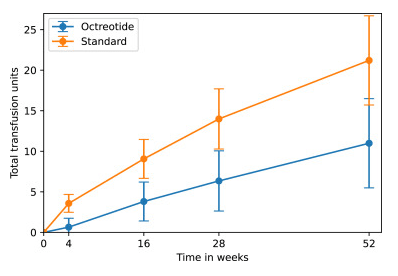
- Suggested dosing for octreotide/somatostatin: 2 mcg/kg bolus then 1-2 mcg/kg/hr (typically max 100 mcg/hr), antibiotics
- Most patients do not require emergency overnight endoscopy.
- Sclerotherapy and banding reviewed -including complications.
- Transjugular intrahepatic portosystemic shunts (TIPS) and Surgical options briefly discussed
The Dreaded Wake-Up Call (Part B) –Lee Bass (Children’s Hospital of Chicago) (pg 67 in syllabus)
Nonvariceal GI Bleeding Management
- Start with ABCs -airway, breathing, cardiovascular –fluid resuscitation/blood products
- Restrictive transfusion strategy (Hgb <7 as threshold) (Villanueva et al NEJM 2013) helpful for survival in adults
- Treatment with PPI improves rates of high risk stigmata on endoscopy
- Prokinetics can improve identication of bleeding lesions
- Preparation for endoscopy is most important (slide on page 70 of syllabus)
- Also on page 70, pictures of typical findings with GI bleeding: nonbleeding vessel, adherent clot, spurting blood, oozing blood, and flat pigmented spot and clean base
- Endoscopic management -combination of two techniques appears to be more effective than single method. injection, thermal probe, hemoclips, hemospray (not available in U.S.
Endoscopic Interventions for Biliary Tract Disease — Victor Fox (pg 75 in Syllabus)
Choledocholithiasis is most common need for interventional biliary endoscopy and increasing related to increase risk with increase in obesity.(Buxbaum J. Gastrointest Clin N Am 2013;23:251‐75)
Requires advanced training to achieve high level of skill and experience
- >200 cases needed to achieve selective cannulation required for interventions
- Acquisition and maintenance of skills by pediatricians is controversial
Other points:
Take-home message: Endoscopic biliary interventions are increasingly employed in children with similar safety and technical success as adult patients
Related blog posts:
Disclaimer: These blog posts are for educational purposes only. Specific dosing of medications/diets (along with potential adverse effects) should be confirmed by prescribing physician/nutritionist. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.