Along with Ragh Varier, I had the privilege of moderating a session on new technologies on patient health. Below I’ve included a few slides and some notes; my notes may have errors of omission or transcription.

Chicago

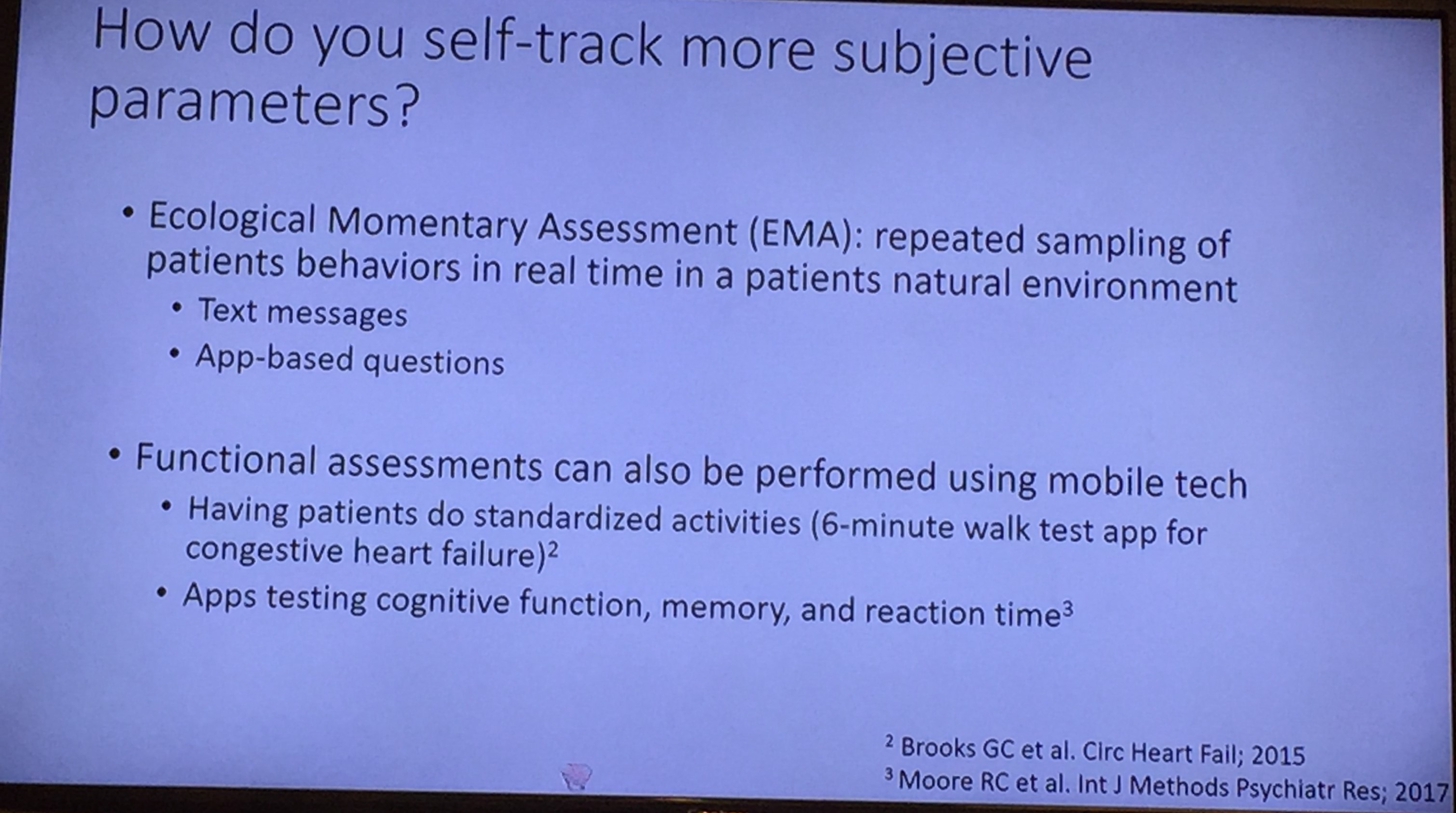
Dr. Mehta’s lecture focused on wearable health technologies. Key points:
- It is already in use in some areas (eg. continuous glucose monitoring for diabetes, ECG sensors).
- She noted that wearable technology dates back to the 1600s with the abacus ring
- Challenges: Accuracy, Actionability/outcome improvement, Reaching at-risk populations (not just the ‘worried well’ populations), regulation, sustainability (users may abandon quickly), and ethical/privacy concerns
- Some families taking technology into their own hands, so to speak. #WeAreNotWaiting. Example: artificial pancreas device system



Dr. Syed’s lecture focused on artificial intelligence in medical-decision making. Key points:
- AI is already in use in areas like facial recognition
- AI may be able to increase polyp detection rate in colonoscopy and improve histology reading
- Her team has been working on using AI to help distinguishing enviromental enteropathy histology from other etiologies
- Other potential uses: AI to help predict Crohn’s disease progression based on histology
Related study (not discussed in talk): Z Deng, H Shi et al. Gastroenterology 2019; 157: 1044-54. The authors collected more than 113 million images from 6970. With a deep-learning algorithm, they found that video capsule endoscopy could have higher detection rates and improved reading time with a “CNN-based” reading system (CNN=convolutional neural network). The mean reading time was reduced from 97 minutes with conventional reading to 6 minutes with CNN-based reading system. The later had 99.88% sensitivity in per-patient analysis (vs. 74.57% with conventional reading).

The oral abstract presentation, by Sonja Swenson, detailed how machine learning was applied to try to improve transplantation selection/PELD scores.
- The authors of this abstract (437) used data from 6273 patients with PELD scores and added additional variables to try to identify a more accurate model.
- Link: All NASPGHAN 2019 Abstracts



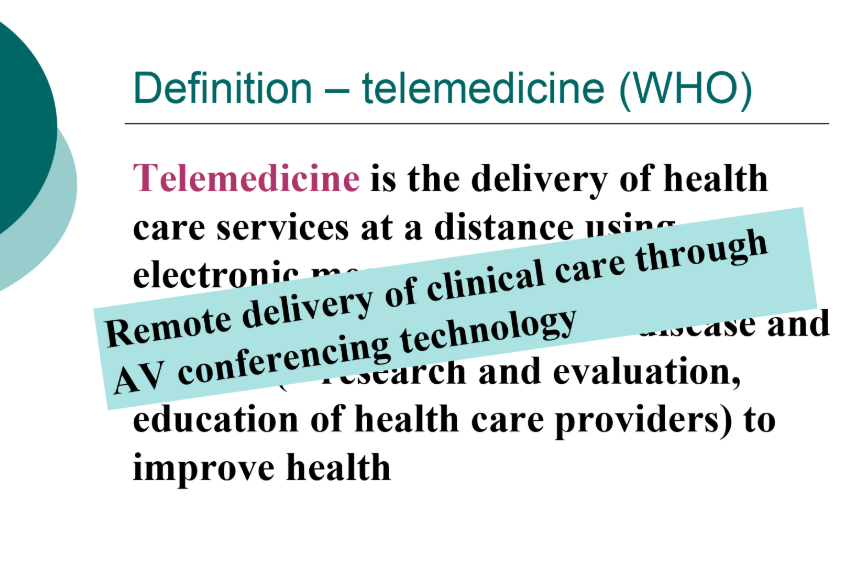
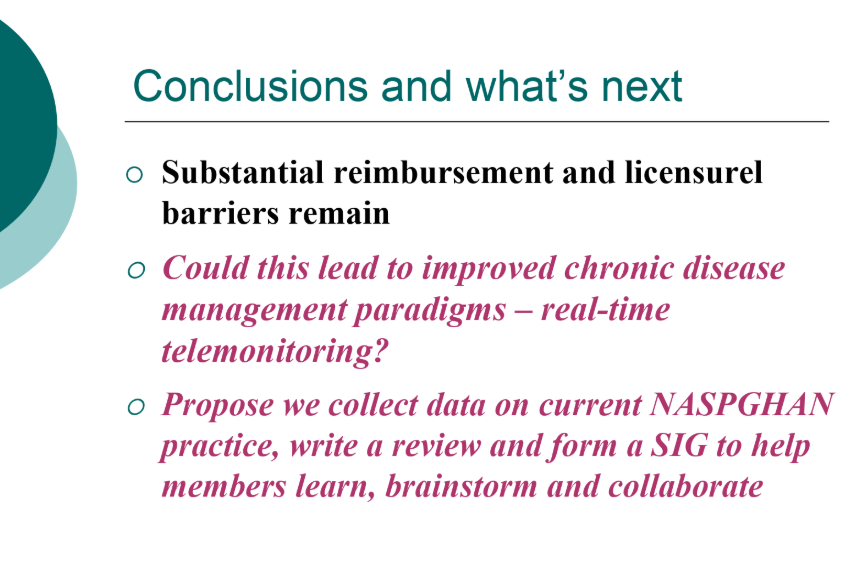
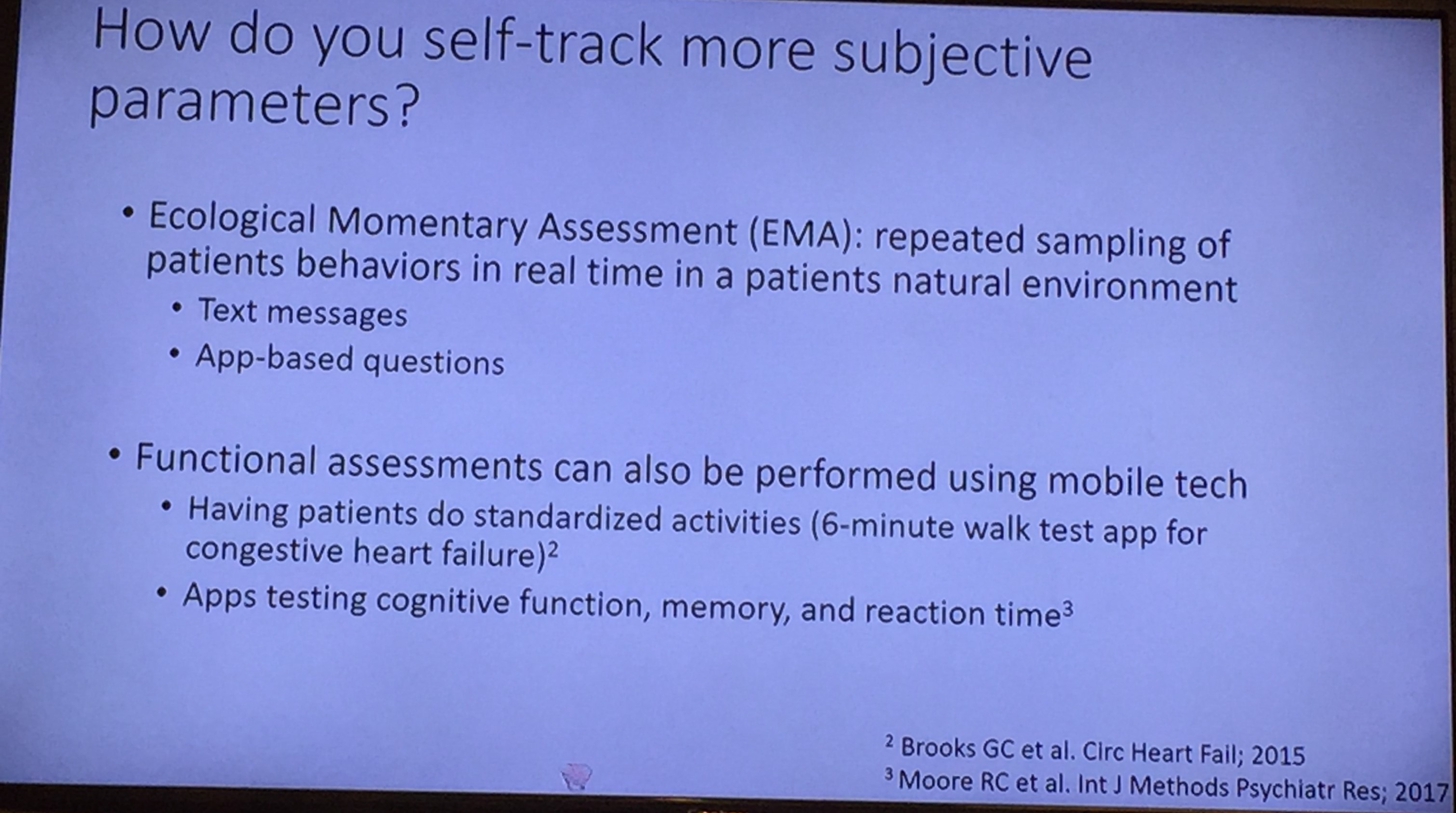
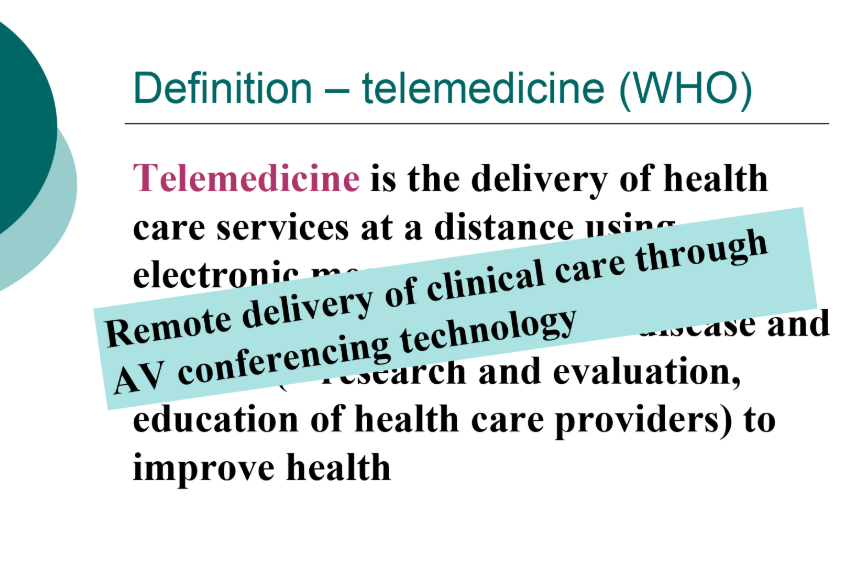
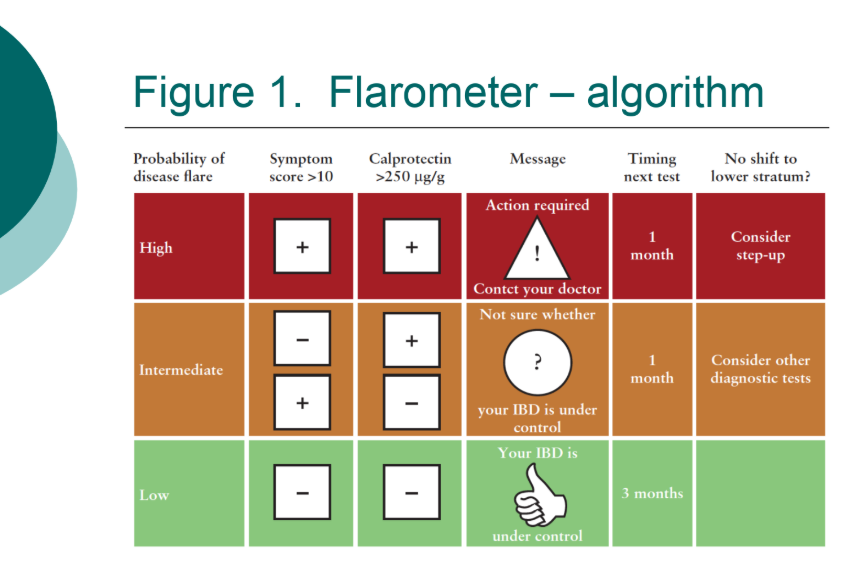
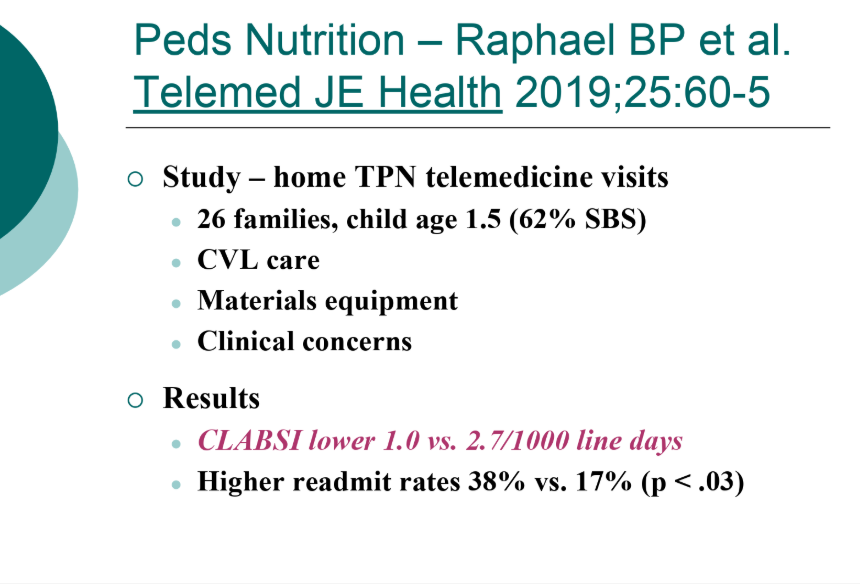
Dr. Li, known by some as the ’emperor of emesis,’ presented a lecture on telemedicine. His full slides: Telemedicine NASPGHAN Updated 2019 (B Li)
Key points:
- When surveyed, patients/families prefer telemedicine over conventional medicine. Key reason is convenience
- Lots of issues from health care provider viewpoint: reimbursement, licensing (improving), increased time
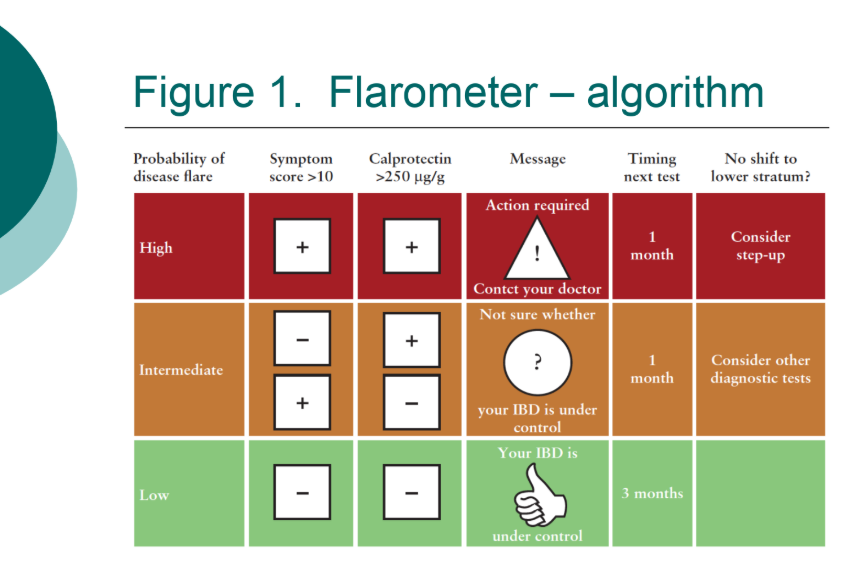
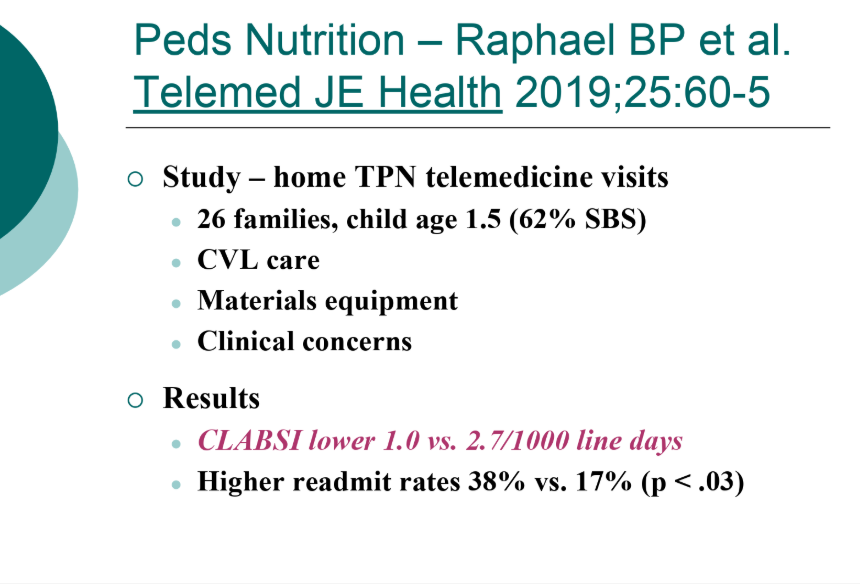
- Many examples of telemedicine/telemonitoring that are ongoing


Disclaimer: NASPGHAN/gutsandgrowth assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. The discussion, views, and recommendations as to medical procedures, choice of drugs and drug dosages herein are the sole responsibility of the authors. Because of rapid advances in the medical sciences, the Society cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. Some of the slides reproduced in this syllabus contain animation in the power point version. This cannot be seen in the printed version.