K Marild et al. Clin Gastroenterol Hepatol 2024; Open Access (PDF)! Association Between Celiac Disease and Irritable Bowel Syndrome: A Nationwide Cohort Study
Methods: Using Swedish histopathology and register-based data, we identified 27,262 patients with CD diagnosed in 2002–2017 and 132,922 age- and sex-matched general population comparators.
Key Findings:
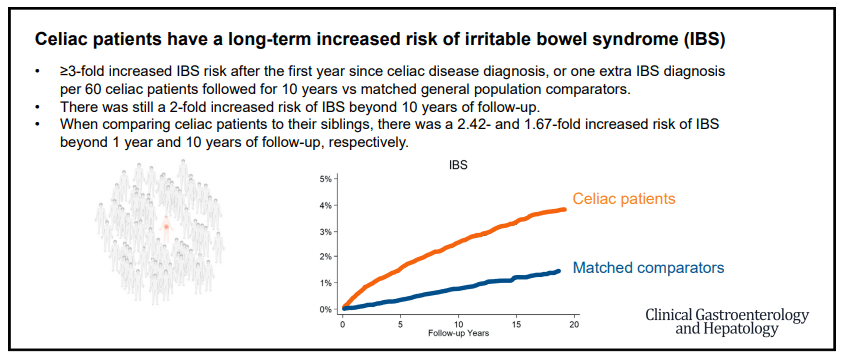
- During an average of 11.1 years of follow-up, 732 celiac patients (2.7%) were diagnosed with IBS vs 1131 matched general population comparators (0.9%).
- Compared with siblings (n= 32,010), celiac patients (n = 19,211) had >/= 2-fold risk of later IBS (aHR, 2.42)
- Compared with celiac patients with mucosal healing, those with persistent villus atrophy on follow-up biopsy were less likely to be diagnosed with IBS (aHR, 0.66)
Interpretation of findings:
“We found celiac patients with persistent villus atrophy on follow-up biopsy less likely to be
diagnosed with IBS than those with mucosal healing. Traditionally, physicians have hesitated to diagnose IBS in patients with an organic gastrointestinal disorder (eg, CD), possibly underestimating the observed IBS risk in CD. This reluctance to diagnose IBS may be particularly true for celiac patients who have not achieved mucosal healing, because persistent villus atrophy may indicate that ongoing symptoms are due to gluten exposure
instead of IBS.”
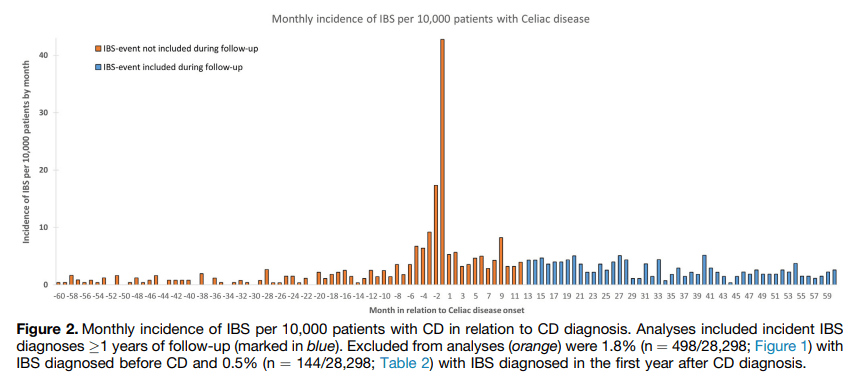
“Surveillance bias is another challenge of studies associating IBS with CD. From the outset of diagnosing and managing these conditions, they are often mutually excluded (eg, CD-specific serology tests are often part of the workup of IBS-like symptoms). Consequently, the
strength of the association between these conditions may be overestimated.” This is why the authors focused on IBS events beyond the first year of CD diagnosis and there continue to be an increased risk of IBS 10 years of follow-up.
Another limitation of this study: “a large proportion of IBS patients are cared for in
primary care or never seek care at all, and hence our study may have had a low sensitivity for IBS, particularly mild IBS.”
My take: While recurrent symptoms in patients with CD could indicate ongoing gluten exposure, recurrent symptoms can also be due to IBS which can occur even with mucosal healing.
Related blog posts:
- Functional Abdominal Pain in Children with Celiac Disease
- Should Patients with IBS be Screened for Celiac Disease?
- IBS Symptoms in Patients with Celiac Disease
- Treatment of Refractory Celiac Symptoms with a Low FODMAP Diet
- How Important is Follow-up in Patients with Celiac Disease
- Work Disability with Celiac Disease
- Celiac Disease: “”80 percent of success is just showing up”
- Improving Care Process in Celiac Disease
- How Slow Do Objective Markers of Celiac Disease Improve
- Followup Biopsies in Pediatric Celiac Disease?