Recently Dr. Arun Singh gave our group a terrific update on Celiac Disease. I have taken some notes and shared some slides. There may be inadvertent omissions and mistakes in my notes.
Key points:
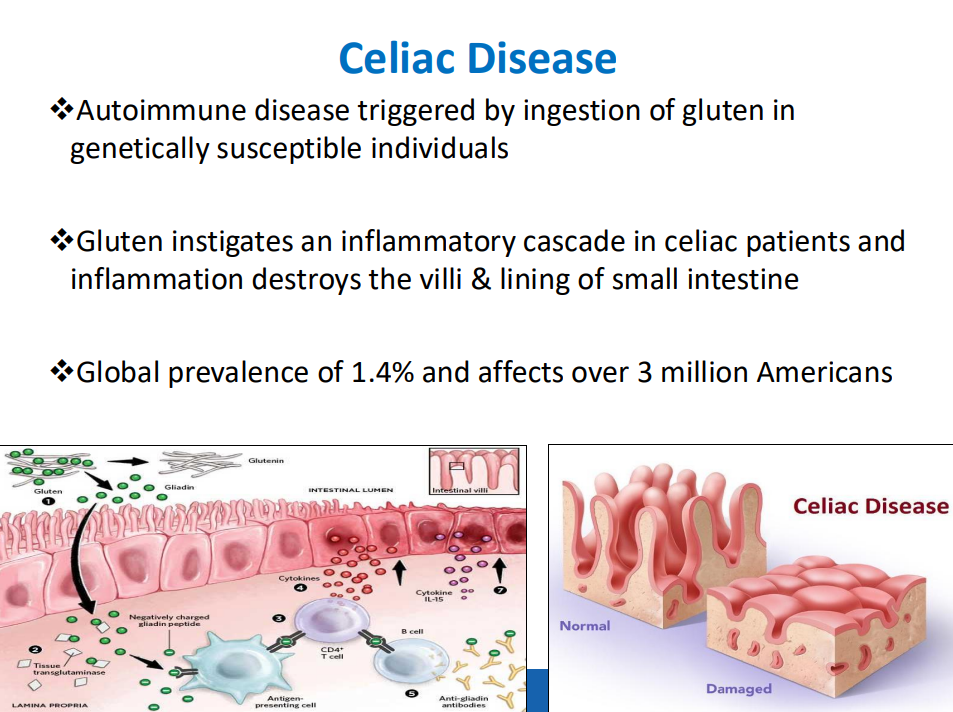
- Celiac disease (CD) global prevalence is about 1.4%, though there are ‘pockets’ with much higher rates (~3% prevalence in Colorado). This equates to more than 3 million Americans with CD
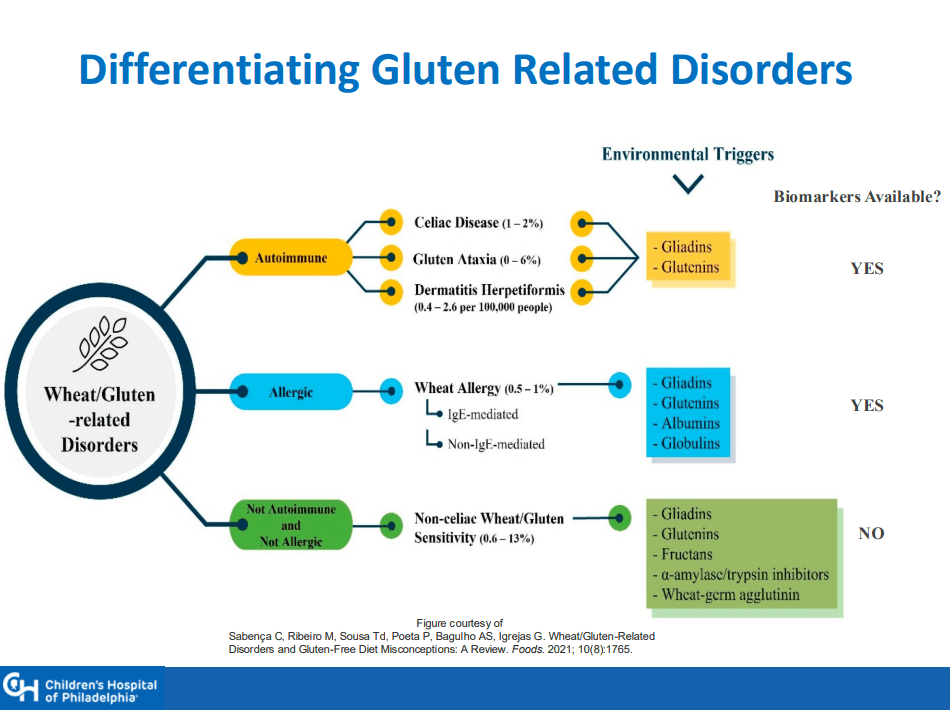
- There is a huge gluten free diet market of ~$7 billion. This market includes CD, nonceliac gluten sensitivity (NCGS) and those with wheat allergies
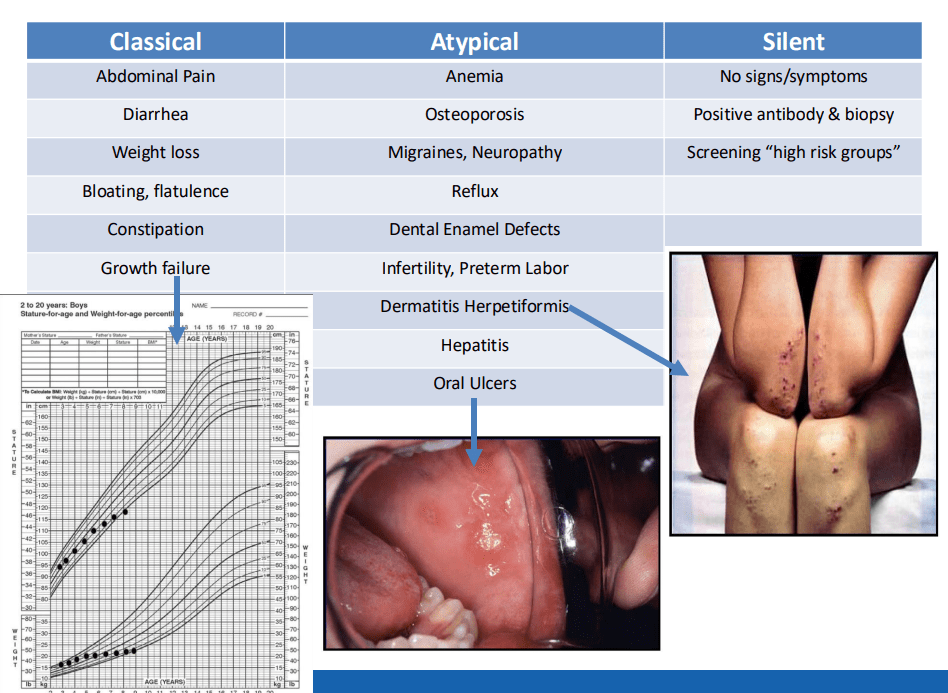
- Many patients have atypical symptoms which can include ADHD, brain fog, headaches, and elevated LFTs. Many have silent CD with no symptoms
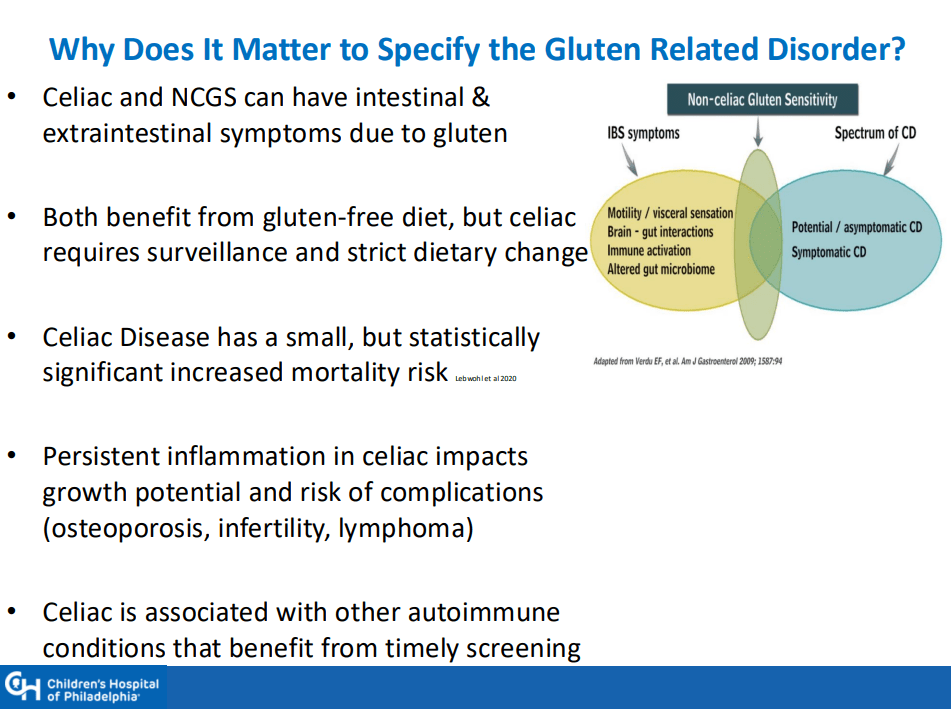
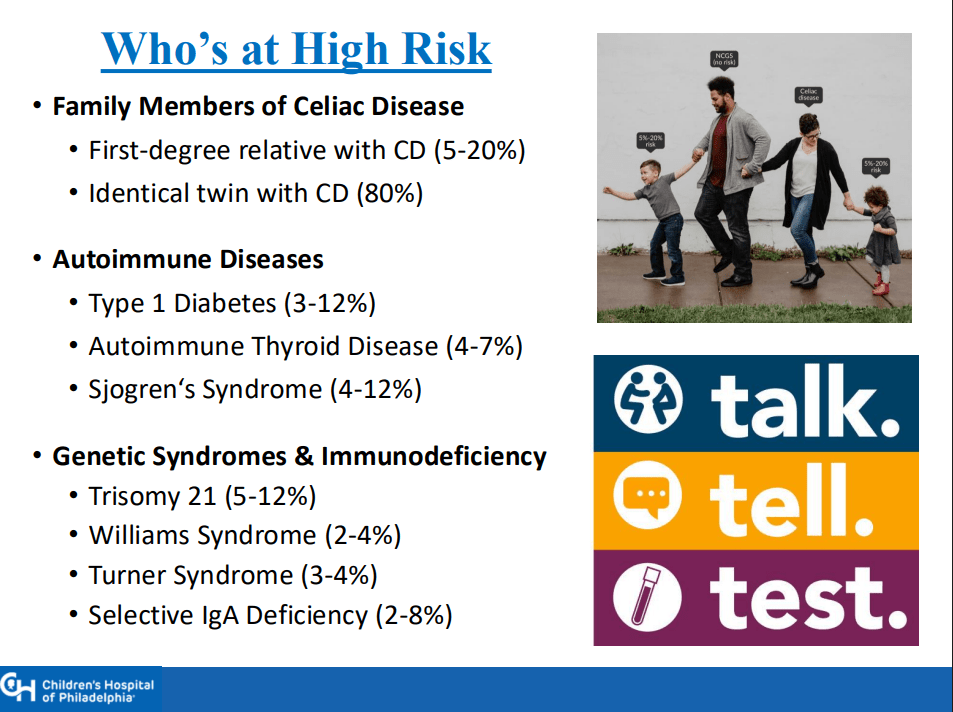
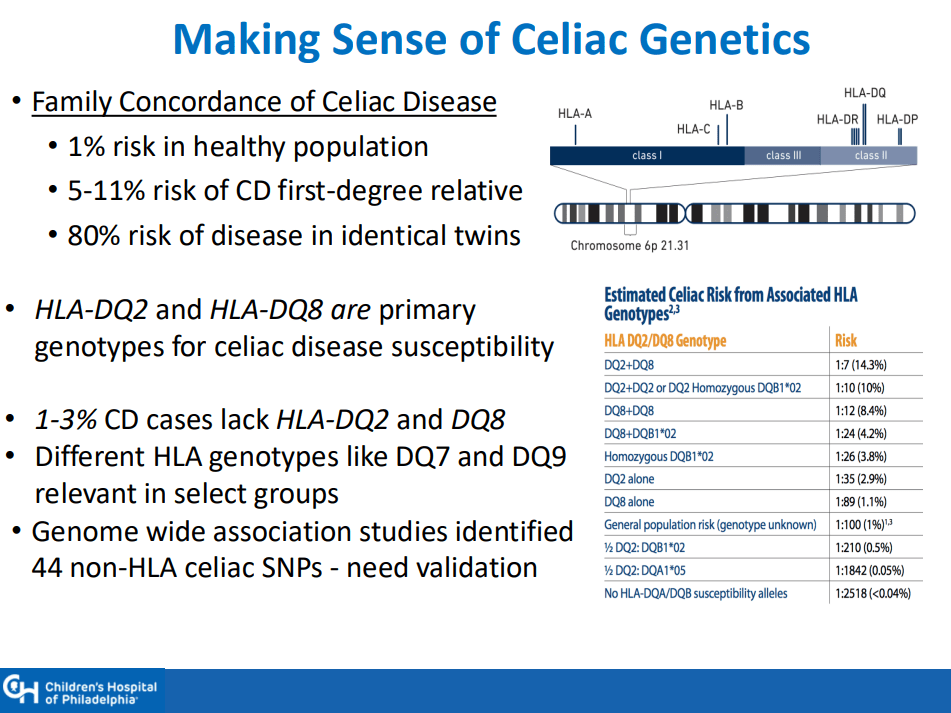
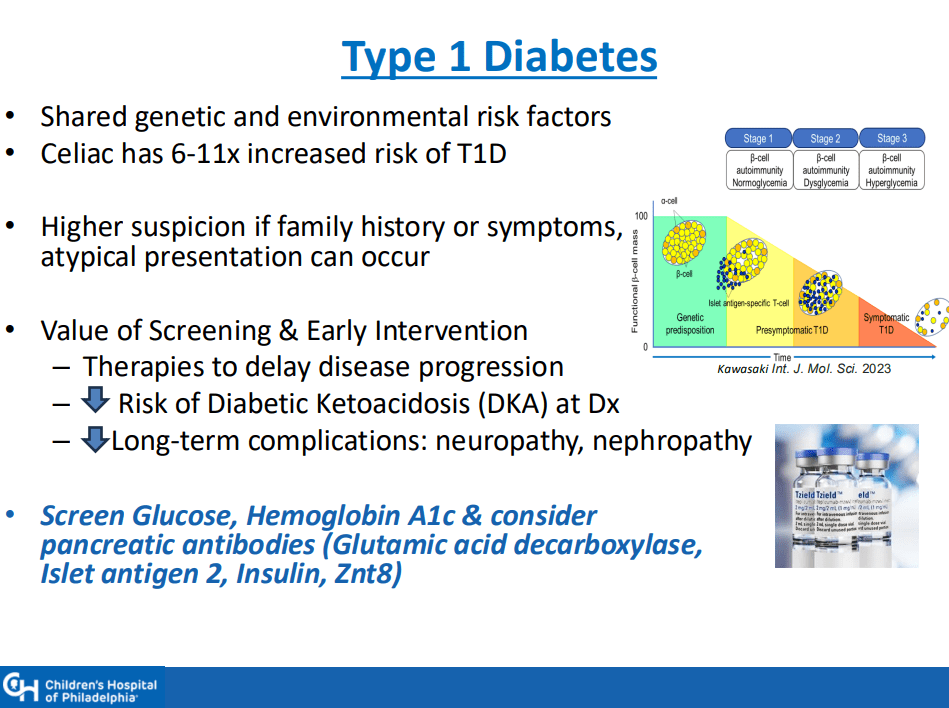
- Higher risk groups include family members (~10% risk for 1st degree, ~80% risk for identical twin), autoimmune diseases (thyroid, diabetes, others), and genetic disorders (Down syndrome, Williams syndrome, Turner syndrome)
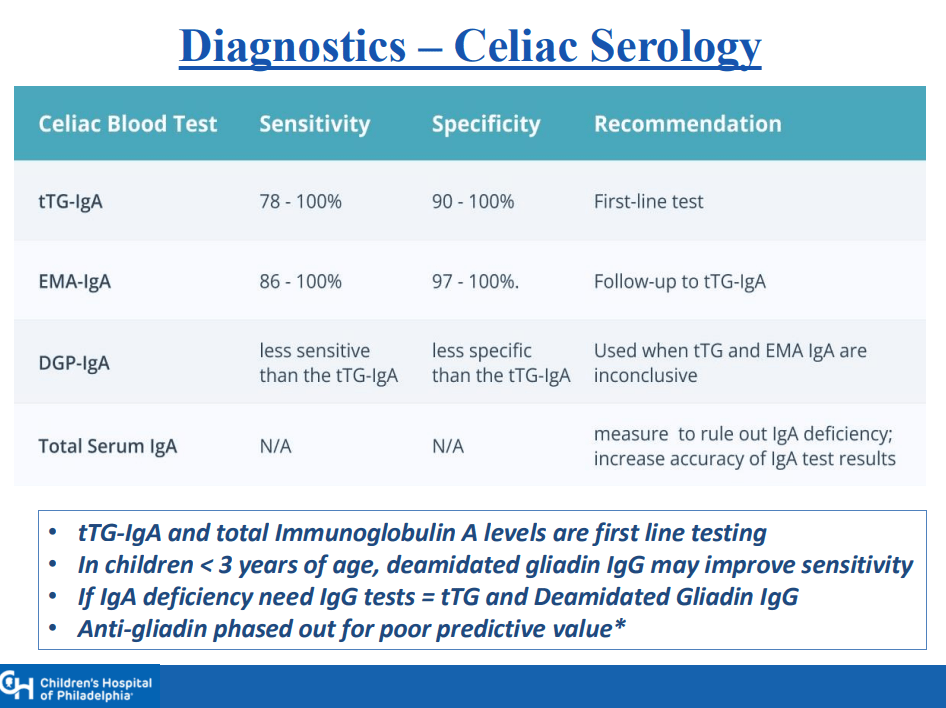
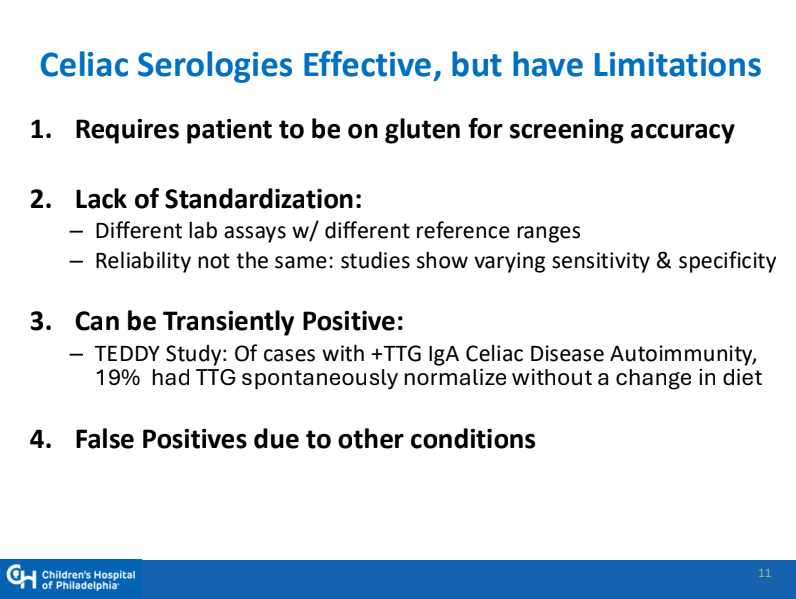
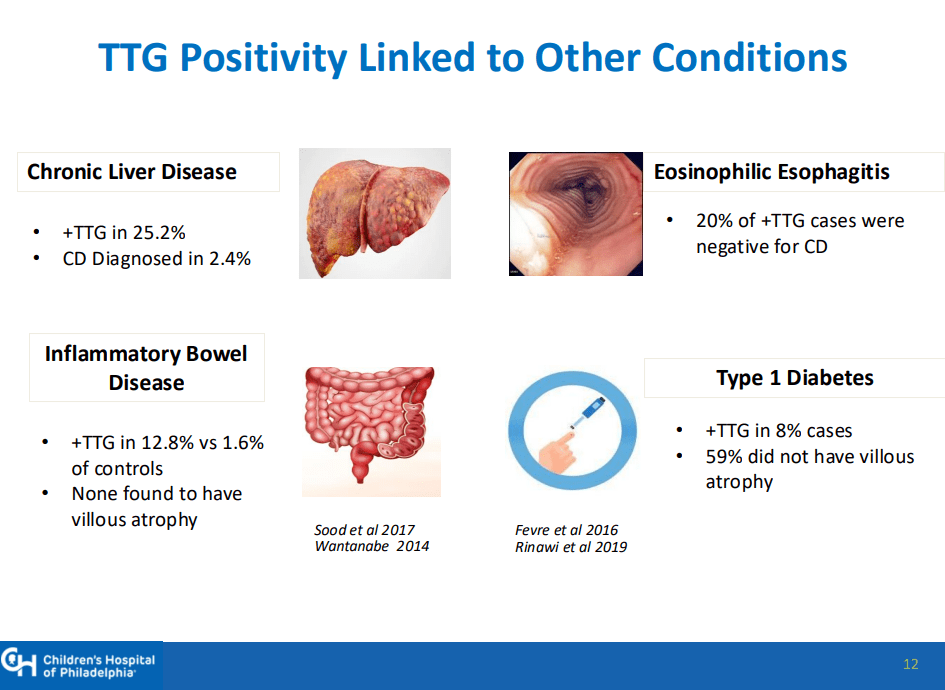
- Transient elevation of TTG IgA is common. In TEDDY study, 19% had TTG IgA spontaneously normalize. Thus, a single abnormal lab is not reliable
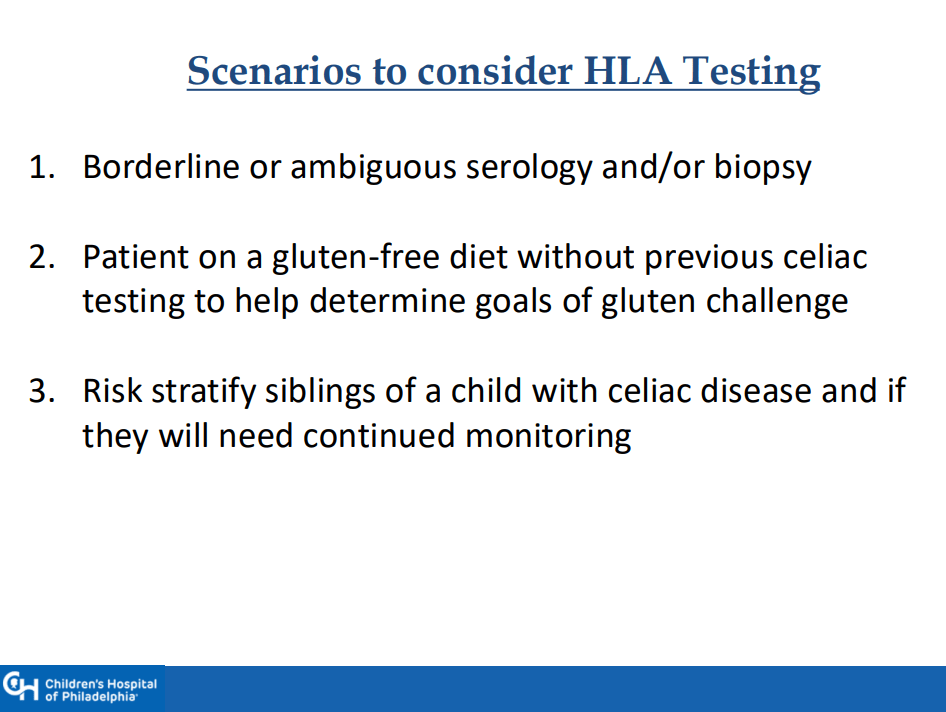
- Genetic testing can be a useful adjunct in a few specific situations, including prior to instituting a gluten challenge
- 1-3% of those with celiac disease may be negative for HLA-DQ2 and HLA-DQ8
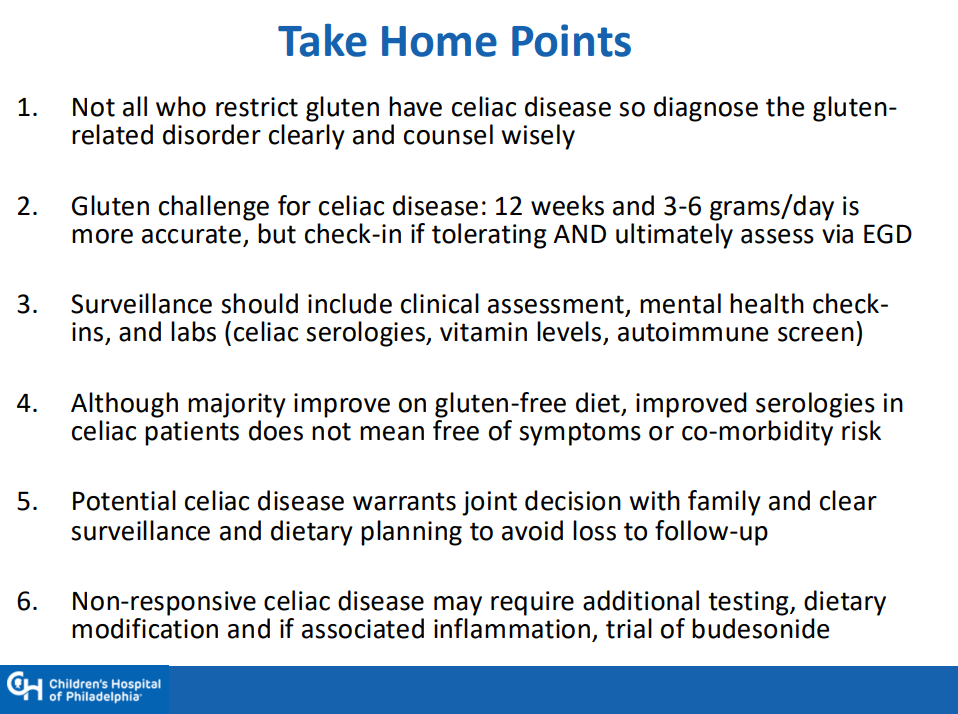
- If a gluten challenge is needed, 12 weeks is ideal. However, if poorly tolerated, then consider endoscopy earlier and Dr. Singh recommends checking in with family 4-6 weeks into the challenge
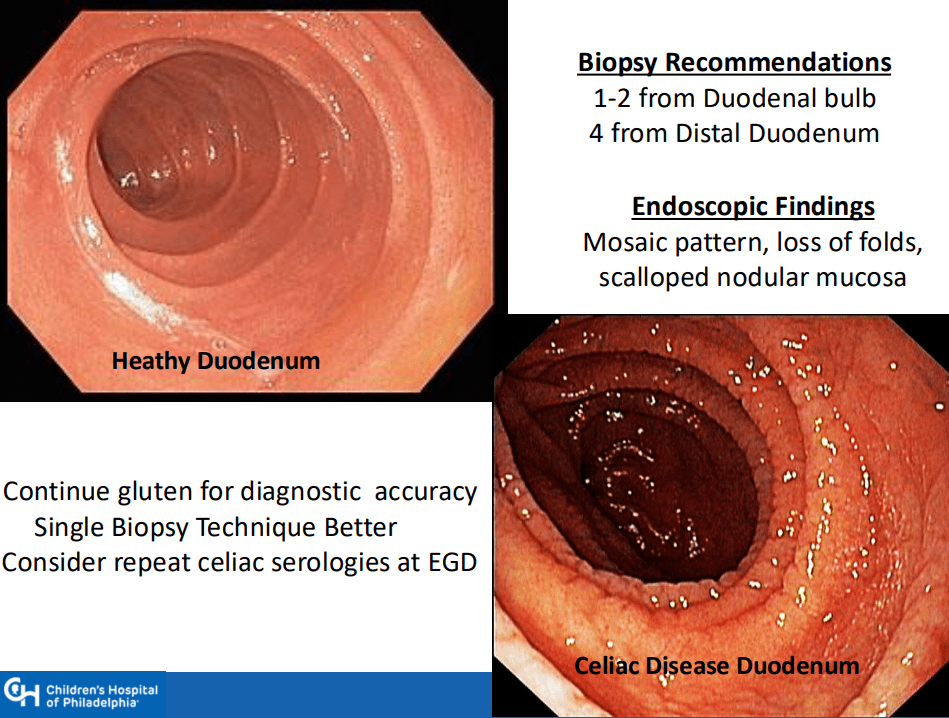
- Endoscopy recommendations: Taking a single biopsy per pass can improve orientation when obtaining duodenal biopsies (bulb and distal portion, 5-6 in total)
- NASPGHAN has not updated comprehensive guidelines for CD in 20 years
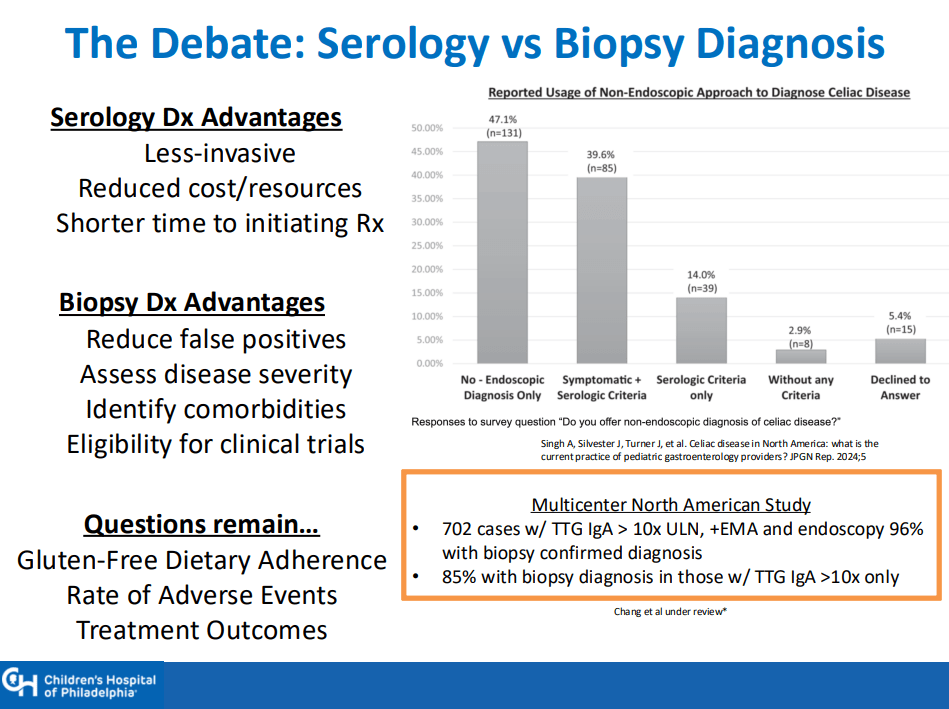
- A survey of NASPGHAN members indicated that ~40% utilize a “no-biopsy” approach in patients. Dr. Singh noted that the accuracy of this approach, based on data from North America, may be about 96%
- Drug trials for CD require a biopsy-confirmed diagnosis
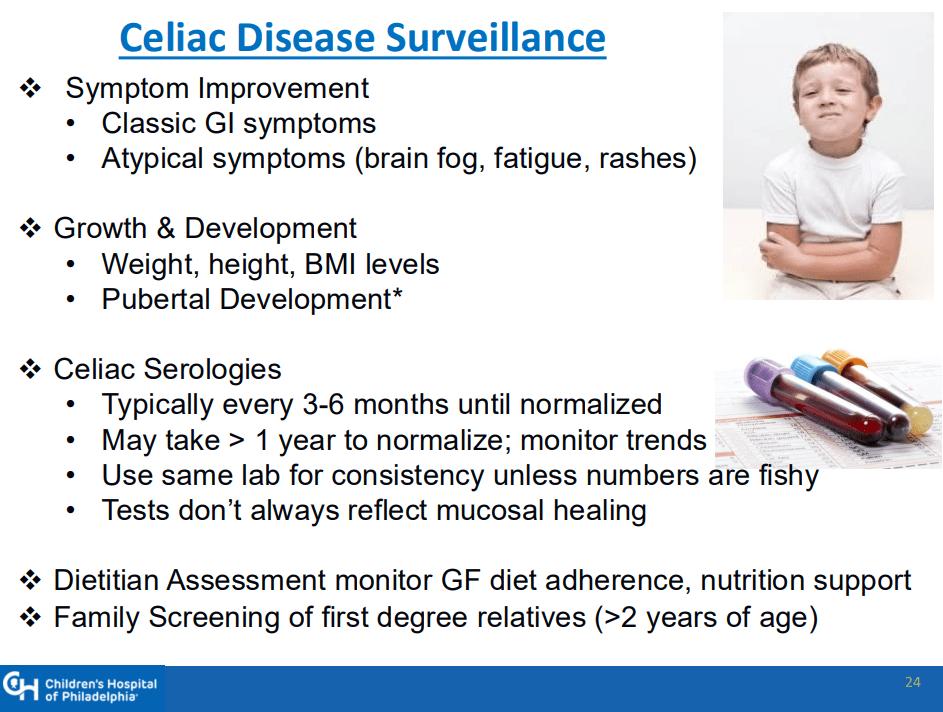
- Surveillance practice is quite variable. Important to follow growth and serology. CHOP approach includes surveillance for type 1 DM
- Followup endoscopy to assess mucosal healing is not the current standard of care but could be helpful in some patients
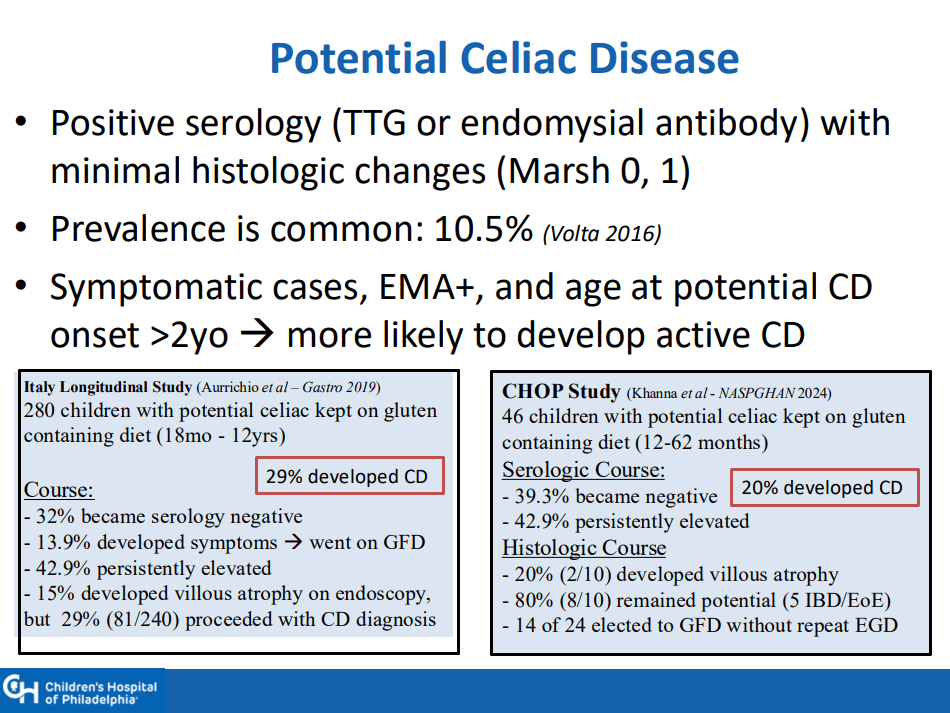
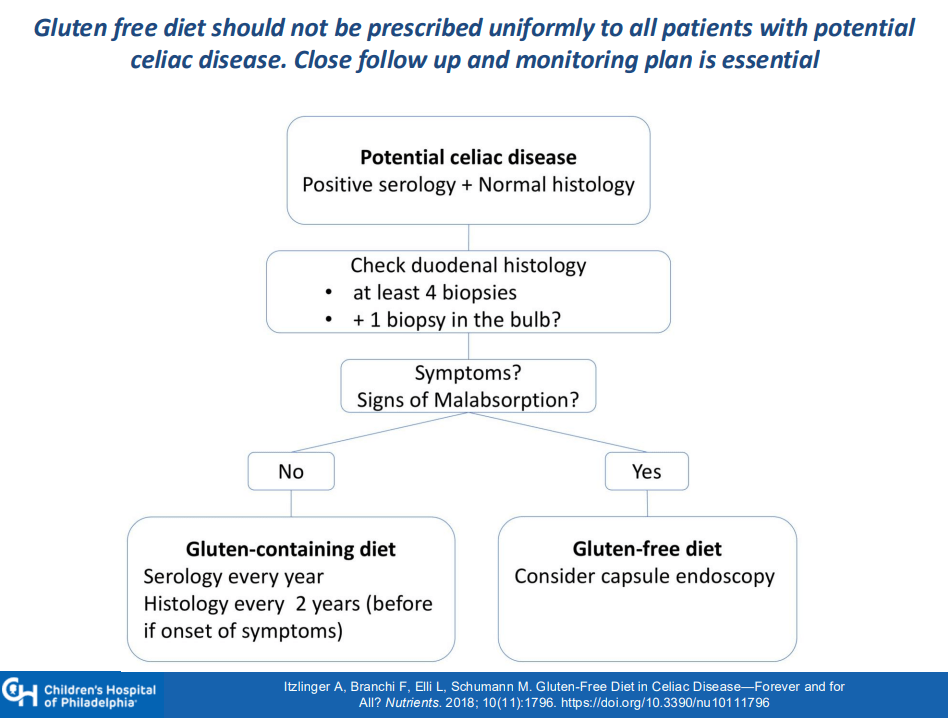
- Among patients with potential CD, about 30% develop CD over time. Thus, these patients should be monitored (yearly labs, f/u scope after 2 years)
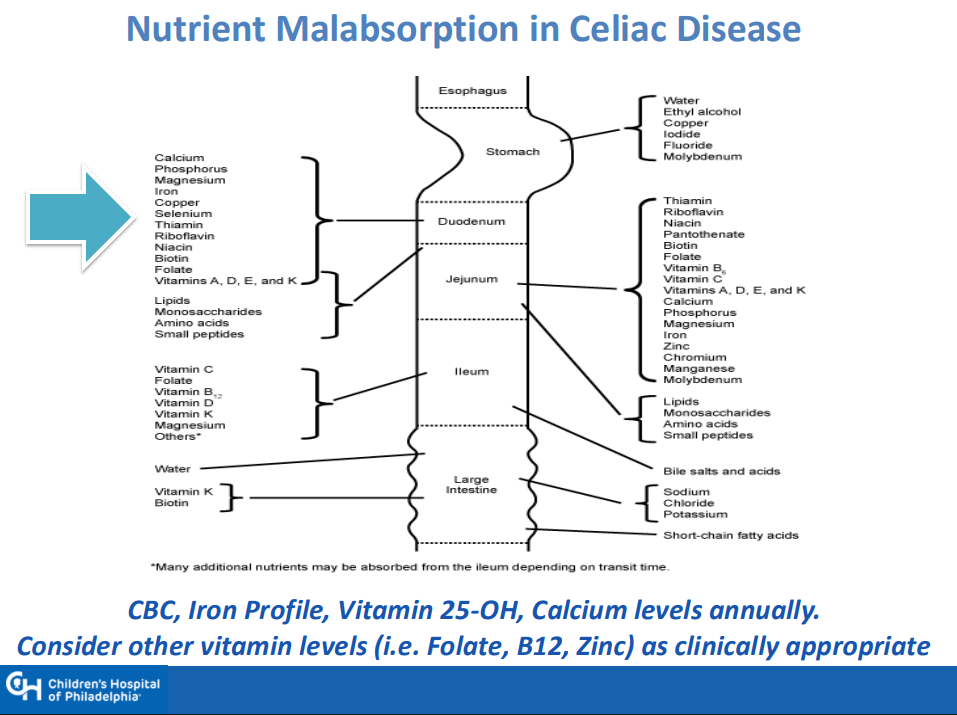
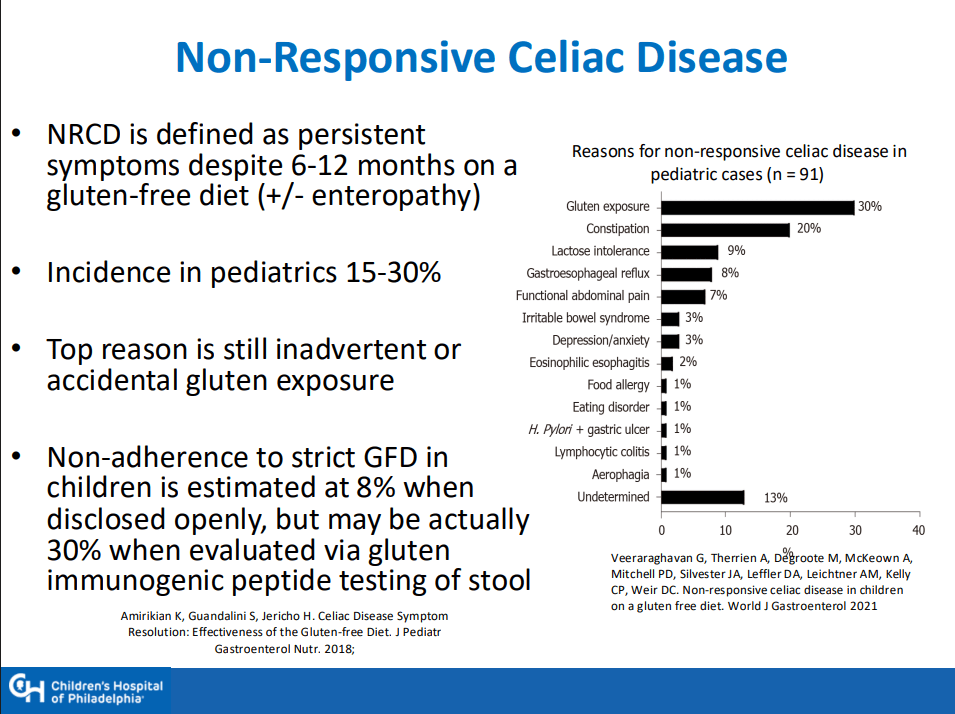
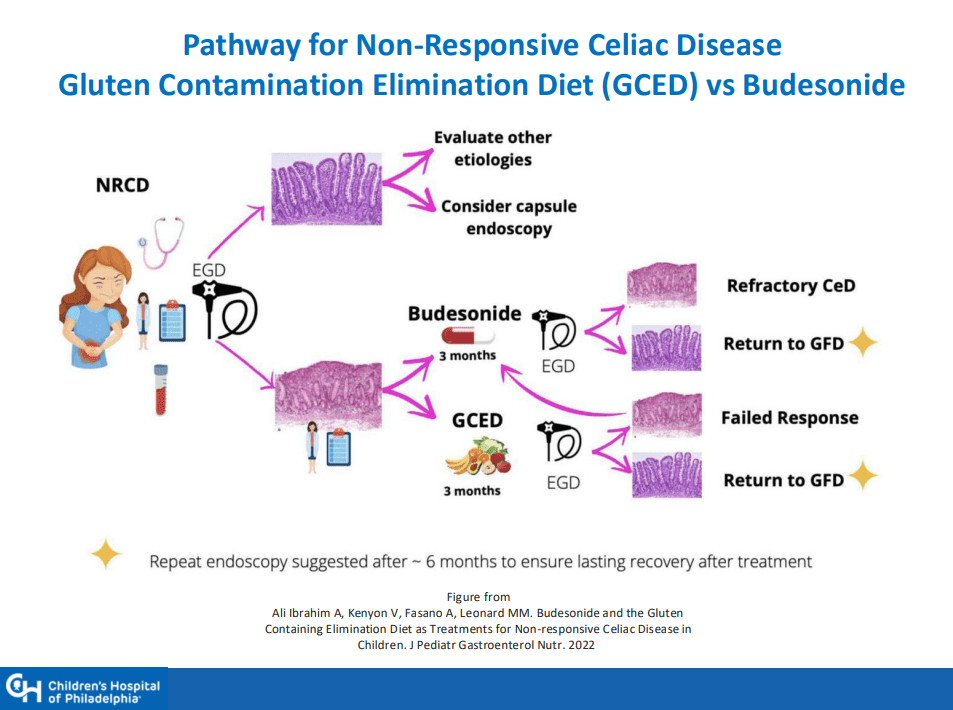
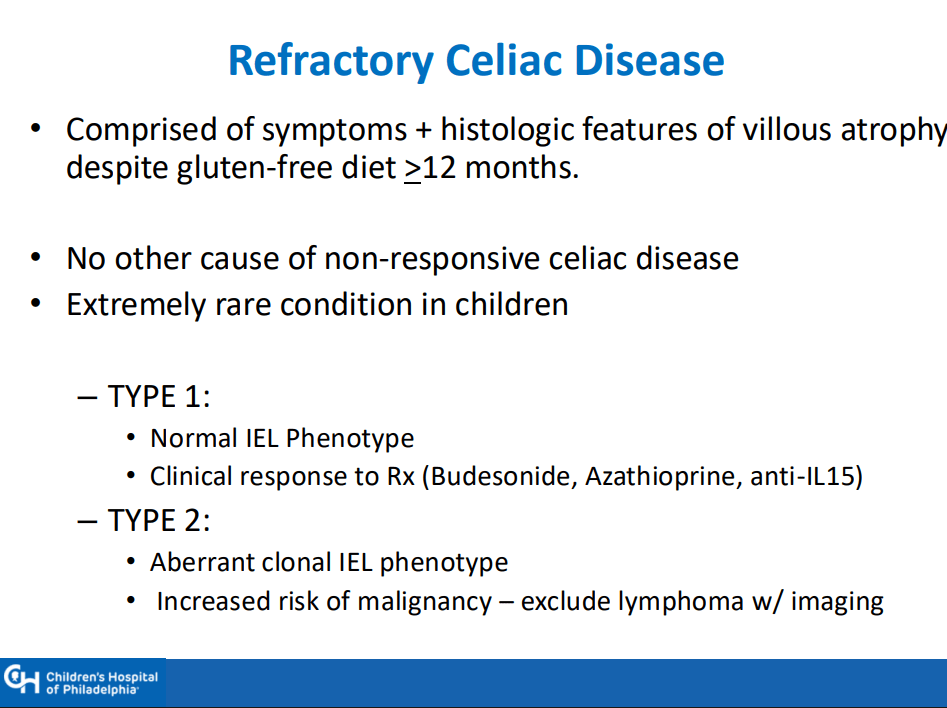
- Nonresponsive/refractory CD: start with nutrition assessment, often needs a f/u scope before consideration of budesonide therapy (9 mg x 12 weeks) or gluten contamination elimination diet

Related blog posts:
- Celiac Disease: Lower TTG-IgA Titers Associated with Isolated Duodenal Bulb Presentation
- What To Do For Pediatric Patients with Non-Responsive Celiac Disease
- Celiac Disease: Pro Tips (Part 1)
- Celiac Disease: Pro Tips (Part 2)
- Celiac Disease: Pro Tips (Part 3)
- Celiac Disease: Pro Tips (Part 4)
- How Many Children with Type 1 Diabetes and High Celiac Titers Have Celiac Disease
- “When is Celiac Disease Celiac Disease?”
- 2023 ACG Celiac Guidelines for Adult and Children
- Taking One ‘Bite’ At A Time -For Celiac Diagnosis | gutsandgrowth
- Celiac Disease: “”80 percent of success is just showing up” | gutsandgrowth
- What To Do For Pediatric Patients with Non-Responsive Celiac Disease
- Treatment of Refractory Celiac Symptoms with a Low FODMAP Diet
- Predicting Risk of Celiac Disease in High-risk Families
- Celiac Advocacy: Food Labeling Modernization Act
- Persistent Villous Atrophy in Celiac Disease Despite a Gluten-Free Diet
- Real-World = Partially-Treated Celiac Disease
- Best Screening For Celiac At All Ages
- Does The Degree of Villous Atrophy Affect Long-Term Outcomes with Celiac Disease? Plus One
- Study May Indicate Biologic Basis for Brain Fog in Persons with Celiac Disease
- @AmyOxentenkoMD: Celiac Disease and Mimics
- 99% Accuracy in Non-Biopsy Diagnosis of Celiac Disease
