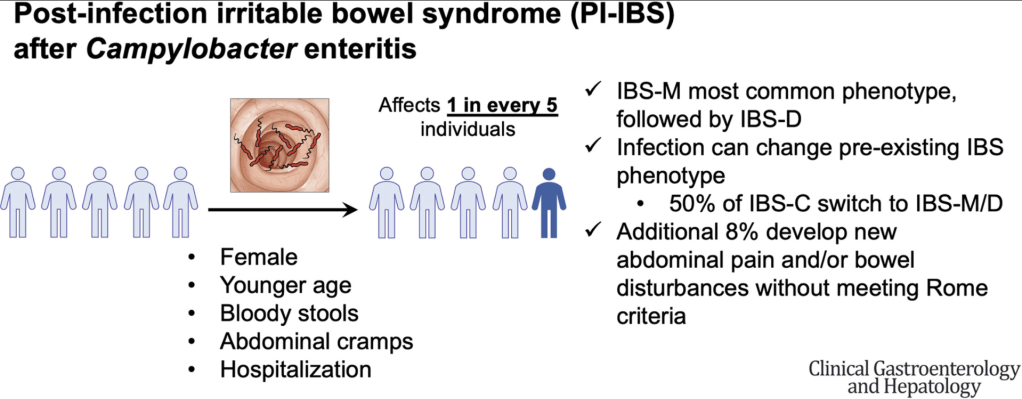
A Berumen et al. Clin Gastroenterol Hepatol 2021; 19: 1855-1863. Characteristics and Risk Factors of Post-Infection Irritable Bowel Syndrome (IBS) After Campylobacter Enteritis
The Minnesota Department of Health collects data on symptoms and exposures upon notification of Campylobacter cases. In this 6-9 month followup survey of 1667 (2011-2019) out of a total of 3586 patients, the authors identified 1418 without preexisting IBS.
Key findings:
- 301 (21%) subsequently developed IBS. Most of these individuals had IBS-mixed (54%), followed by IBS-diarrhea (38%), and IBS-constipation (6%)
- Additionally, the authors note that 121 patients (8.5%) had new GI problems after infection that did not meet thresholds set by Rome criteria
- Among patients with IBS-mixed or IBS-diarrhea before infection, 78% retained their subtypes after infection. In contrast, only 50% of patients with IBS-constipation retained that subtype after infection;40% transitioned to IBS-mixed
- Of patients with pre-existing IBS, 38% had increased frequency of abdominal pain after Campylobacter infection
- One limitation of the study is ‘responder bias.’ There may be a lower rate of IBS/GI symptoms in the subset of patients who did not respond to survey.
My take: A lot of people develop IBS and other GI symptoms after Campylobacter infection; those with IBS often have intensification of their symptoms.
Related blog posts:
- Mechanisms of Postinfectious IBS & Functional Disorders
- Is There a Way to Prove Which Dietary Factors Trigger IBS?
- Clinically Useful Biomarkers for Irritable Bowel Syndrome? | gutsandgrowth
- IBS Subtypes in Pediatrics | gutsandgrowth
- Mechanisms of irritable bowel syndrome
- Ondansetron for Irritable Bowel with Diarrhea? | gutsandgrowth
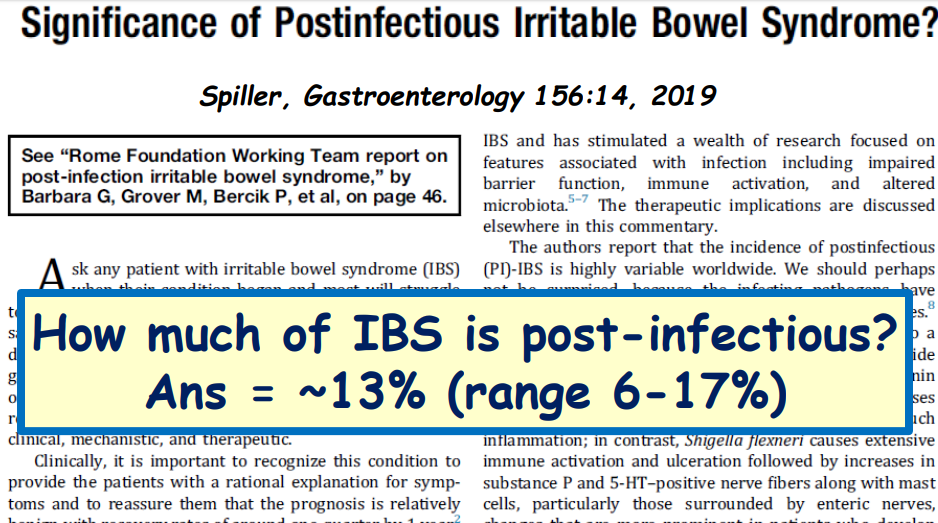
Related study: Am J Gastroenterol 2012 Jun;107(6):891-9. “Norovirus GE leads to the development of PI-IBS in a substantial proportion of patients (13%), similar to that reported after bacterial GE.”