KL Karunungan et al. Liver Transplantation 20021: 27: 200-208. Impact of Payer Status on Delisting Among Liver Transplant Candidates in the United States
This was a retrospective study which relied on large national databases.
- The 1‐year cumulative incidence of delisting was 9.0% (95% confidence interval [CI], 8.3%‐9.8%) for patients with private insurance, 10.7% (95% CI, 9.9%‐11.6%) for Medicare, and 10.7% (95% CI, 9.8%‐11.6%) for Medicaid
- Medicare (HR, 1.20; 95% CI, 1.17‐1.24; P < 0.001) and Medicaid (HR, 1.20; 95% CI, 1.16‐1.24; P < 0.001) were independently associated with an increased hazard of death or deterioration compared with private insurance.
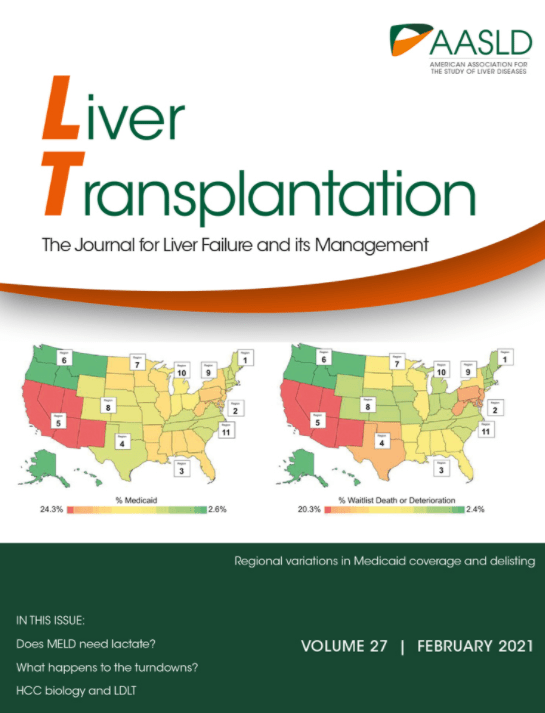
- The article highlights regional variation in payor coverage and change in watilist death or deterioration from 2002-2018 (Figure 1)
- Higher levels of education and employment were protective against waitlist mortality and deterioration
- Female sex was a risk factor for delisting which may be in part to body size as women are more likely to have an organ declined as a result of small stature
L China et al. NEJM 2021; 384: 808-17. A Randomized Trial of Albumin Infusions in Hospitalized Patients with Cirrhosis This was the ATTIRE trial; somehow ATTIRE is an acronym to allude to “Albumin to Prevent Infection in Chronic Liver Failure.” This trial was a multicenter, randomized controlled study.
“In patients hospitalized with decompensated cirrhosis, [daily] albumin infusions to increase the albumin level to a target of 30 g per liter or more was not more beneficial than the current standard care.” The standard of care included giving albumin under specific circumstances: large volume paracentesis, spontaneous bacterial peritonitis, or hepatorenal syndrome. Infusions (20% albumin) were infused at a rate of 100 mL/hr. In addition, the albumin group, which received 10 times as much albumin as the standard group, had more severe or life-threatening adverse events, especially pulmonary edema or fluid overload.
F Wong et al. NEJM 2021; 384: 818-828. Terlipressin plus Albumin for the Treatment of Type 1 Hepatorenal Syndrome In this multicenter, randomized controlled study, terlipressin was associated with improved renal function -reversal of HRS occurred in 32% compared to 17% in placebo group; however, it was associated with increased serious adverse events (eg. respiratory failure) and increased death (51% vs 45% in placebo group).
ER Perito et al. JPGN 2021; 72: 417-424. A Learning Health System for Pediatric Liver Transplant: The Starzl Network for Excellence in Pediatric Transplantation The Starzl Network for Excellence in Pediatric Transplantation (SNEPT) is the first multicenter effort by pediatric liver transplant teams. Its goal is to establish and share evidence-based care to improve liver transplantation outcomes. If successful, SNEPT should be to liver transplantation as ImproveCareNow network is for pediatric inflammatory bowel disease.
