JS Khoo et al. J Pediatr Gastroenterol Nutr. 2025;80:611–616. Impact of diagnostic testing on outcomes of children with rumination syndrome
Background: “A prior study from our institution showed that many patients undergo extensive diagnostic testing, which is associated with high financial cost with low clinical yield and delay in diagnosis.”
Methods: This was a retrospective study with 152 children (60% female, median age of diagnosis 13 years) with rumination syndrome (RS). 22 patients (14%) had diagnostic testing that confirmed RS.
Key findings:
- The confirmatory testing group was more likely to need supplemental nutrition (p ≤ 0.001) and to receive intensive treatment (68% vs 24%) (p < 0.001)
- After treatment, the proportion of patients without vomiting increased in both groups without a statistically significant difference between the two groups or needing supplemental nutrition.
Discussion Points:
“Our findings reveal that despite advancements in testing methodologies, undergoing diagnostic testing and receiving a positive result for RS is not associated with improved outcomes, specifically in cessation of vomiting, after treatment. In situations where patients and caregivers have difficulty accepting the clinical diagnosis, selective testing may be justified as acceptance of the diagnosis is a crucial aspect of the therapeutic plan for all gut-brain interaction disorders.”
Limitations included selection bias. While there were not overt differences in outcomes, the confirmatory testing group required more intensive treatment. As such, the testing may have some benefit in this group (though this was not identified in this retrospective study).
My take (borrowed in part from the authors): “We recommend that clinicians avoid diagnostic testing in children who clearly meet symptom-based criteria for RS and accept the diagnosis.”
Related blog posts:
- Potential Bias with Interpreting Rumination Outcomes
- Most Kids with Rumination Respond to Specialized Treatment
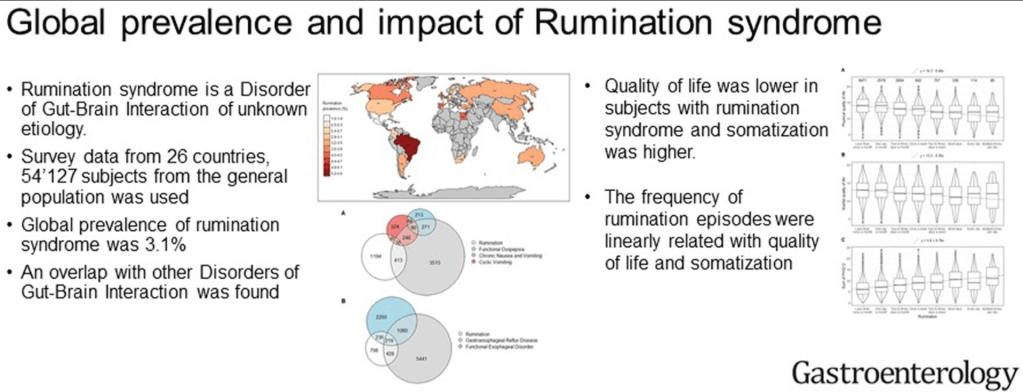
- Internet Survey: Lots of People Have Rumination
- Expert Advice for Diagnosis and Treatment of Rumination Syndrome
- High-resolution Esophageal Manometry for Rumination Syndrome.
- Costs of Rumination (You don’t have to be Vinny Gambini to make the diagnosis)
- Jose Garza: What’s New in Motility (Part 2)
- Jose Garza: What’s New in Motility (Part 1)

There is a blue heron about to take flight due to the oncoming train