J-W Yang et al. Gastroenterology, Volume 169, Issue 5, 958 – 969.e5. Open Acces! Efficacy of ACupuncTure in Irritable bOwel syNdrome (ACTION): A Multicenter Randomized Controlled Trial
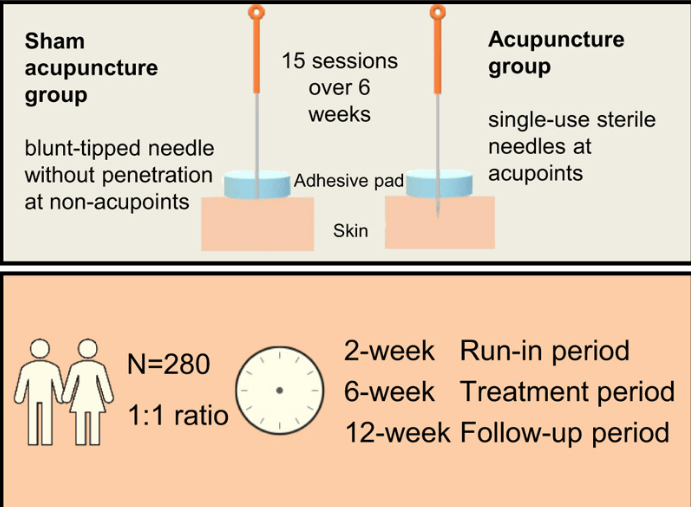
This ACTION study enrolled 280 patients (18-75 yrs) with IBS-D in a multicenter randomized controlled trial in 6 hospitals in China. “For the sham acupuncture group, blunt-tipped placebo needles with a similar appearance to real needles were used over the adhesive pads with no skin penetration. Five fixed pairs of non-acupoints (10 stimulation points in total) away from meridians or conventional acupoints were used.”
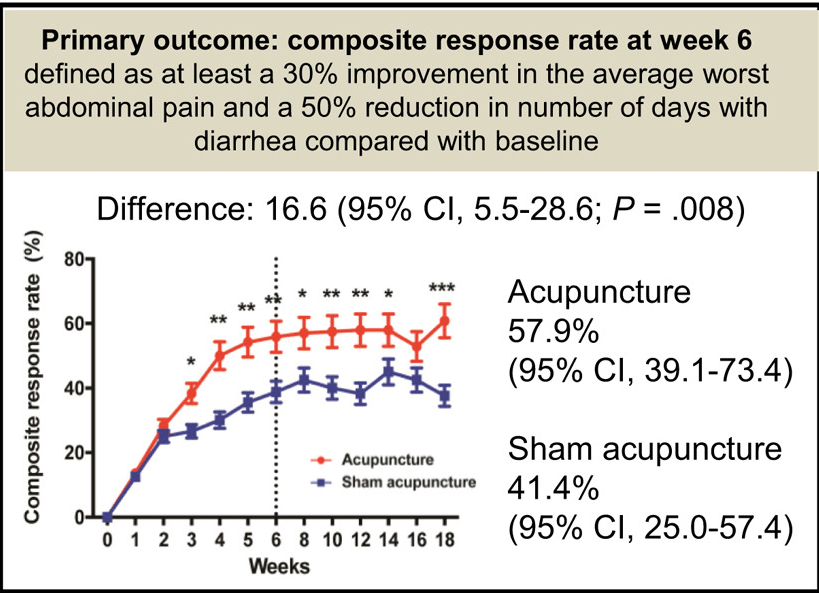
Key finding:
- The primary outcome (see below) was reached by 71 (57.9%) patients in the acupuncture group compared with 47 (41.4%) patients in the sham acupuncture group (risk ratio 1.40; P = .008)
- The effects of acupuncture in symptomatic improvements of IBS-D persisted 3 months after treatment with minimal to no side effects
- Limitations including the difficulty of acupuncture blinding (despite the identical treatment setups)
My take: Acupuncture, especially given its safety, is a reasonable therapy for IBS-D; though, it is not recommended in recent pediatric guidelines. “The rub” in many locations is finding qualified practitioners.
Related blog posts:
- Treatment Guidelines for Pediatric Irritable Bowel Syndrome
- “How to Approach a Patient with Difficult-to-Treat IBS”
- IBS Impact: Survey Reveals Daily Life Struggles
- Acupuncture for irritable bowel syndrome (2012). In this study, true acupuncture was not shown to be more effective than sham acupuncture; however, there was a high placebo response with sham acupuncture
- Enhanced Placebo Effect For Irritable Bowel Syndrome and Functional Abdominal Pain in Adolescents
- “Implementing psychological therapies for gastrointestinal disorders in pediatrics”
- Cognitive Behavioral Therapy for Childhood Abdominal Pain | gutsandgrowth
