SH Ibrahim et al. Hepatology 2020; 71: 1474-85. Thorough review of liver diseases in the perinatal period and relationship of the maternal-infant interactions. Liver diseases discussed include GALD which has “strikingly normal or near normal transaminases” despite liver failure (most common etiology). Treatment for GALD includes IVIG (1 g/kg) along with subsequent double-volume exchange transfusion. The review covers maternally-transmitted viral infections, fatty liver disease, and acute fatty liver disease of pregnancy (AFLP); AFLP is most commonly caused by LCHAD but can be caused by other defects in fatty acid oxidation.
RT Khalaf, RJ Sokol. Hepatology 2020; 71: 1486-98. This review focuses on intestinal failure-associated liver disease (IFALD). The review provides an in-depth discussion of intravenous lipid emulsions and other factors implicated in the pathogenesis.
- Risk factors: bacterial overgrowth, central line infections, recurrent sepsis, prematurity, parenteral nutrition composition, and micronutrient imbalances
- Protective factors: early enteral nutrition, cycled parenteral nutrition, glucagon-like peptide 2, preservation of ileocecal valve, small bowel lengthening when appropriate
- While the authors acknowledge that lipid minimization often improves cholestasis, they advise caution due to concern for both essential fatty acid deficiency and detrimental effects on brain growth.
- Prevention of central line infections with use of ethanol locks is important and effectively reduces the rate by more than 80% (though currently costs of ethanol locks have skyrocketed: FDA Safety Initiative Complicit in Ethanol Costing $30,000 for 1 oz)
- The authors note that long-term survival from intestinal transplantation is only 40% at 10 years indicating benefit of ongoing parenteral nutrition management if feasible.
Related blog posts:
PL Valentino et al. JPGN 2020; 70: 547-54. This article discusses potential management of Wilson disease diagnosed in infancy based on ATP7B genetic testing. Very little evidence presented. Suggests starting Zinc therapy at an early age and monitoring for copper deficiency along with efficacy. More precise recommendations regarding urine copper goals for children would be helpful as well.
Large (n=112, median age 38 years) prospective observational study of Acute Hepatic Porphyria. L Gouya et al. Hepatology 2020; 71: 1546-58. Key findings from EXPLORE group:
- Chronic symptoms were noted in 65%; 46% had daily symptoms. Symptoms including body pains, trouble sleeping/tiredness, anxiety, GI symptoms (eg. nausea) and weakness.
- During the 2-year study period, 88% experienced a total of 483 attacks; 77% of these attacks required treatment at a health care facility or hemin administration
- Median annualized attack rate was 2.0
- UrineDelta-aminolevulinic acid (ALA) and porphobilinogen (PBG) compared with upper limit of normal at baseline and increased further during attacks.
- At baseline, 16% had elevations of liver aminotransferases
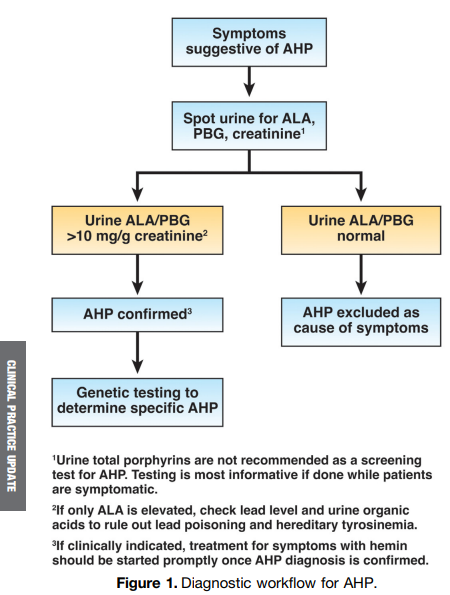
- Related reference: M Balwani et al. Hepatology 2017; 66: 1314-22. Acute Hepatic Porphyrias -Review. Current recommendations include gene sequencing to confirm all biochemical cases. Biochemical tests are spot urine testing of porphobilinogen (PBG), 5-aminolevulinic acid (ALA), and porphyrins. A normal urine PBG in symptomatic patients “excludes the three most common acute hepatic porphyrias.” For those with abnormal studies, this reference is a handy.
Automated ascites pump. F Wong et al. Liver Transplantation 2020; 26: 651-61. In this study with 30 patients, interventional radiology placement of an “alfapump” helped manage refractory ascites in cirrhosis.

Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition