There has been a lot of hype about the benefits of a high protein diet. In a recent substack article (8/31/25) , Eric Topol reviews the data on this (for adults).
Here’s the link:Our Preoccupation With Protein Intake
Key points:
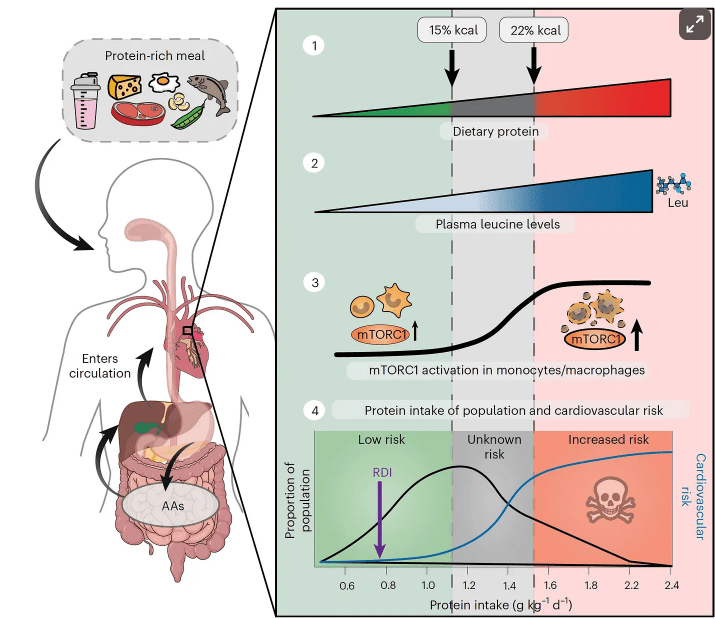
- An important study in both mice and people, demonstrating that high protein intake accelerated atherosclerosis and increases cardiovascular risk (see figure below). “The increased risk of atherosclerosis and cardiovascular disease from the data, showing up at protein intake of 1.5 g/kg/day.”
- “The pervasive call for higher protein intake stems from the assertion that people are not getting adequate amounts in their diet, namely the 0.8 g/kg/day recommend by the National Academy of Medicine and the World Health Organization….
- Regarding the need to increase protein intake 2-3 fold per day, Stuart Phillips, a leading expert on protein, energy, and building muscle mass, who is a professor at McMaster University in Canada, said “It’s baloney. But there’s a generation, particularly young men, and now an increasing number of young women, who are absolutely brainwashed by what they hear online”…there are no data to support more than 1.6 g/kg/day of protein intake.
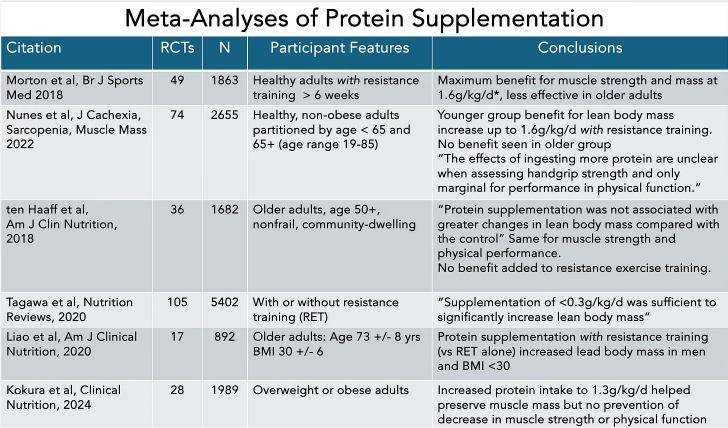
- “What about the strong recommendation for high protein in older adults? In the 50+ group, as reviewed by ten Haaf and colleagues, the randomized trials show no benefit of high protein on top of resistance training compared with resistance training alone (the control group) for improved lean body mass” [in 12 trials]
- “85% of the US population consumes more than the 0.8 g/kg/day recommended daily intake (RDI) and nearly 25% are consuming twice the RDI“
Safety concerns:
- “There are many observational studies that have raised the safety concerns for high-protein intake, particularly derived from animal protein, for increased risk of type 2 diabetes, cardiovascular disease, and higher all-cause mortality. A prospective study of ~44,000 women in Sweden followed for 15.7 years found an association of high-protein diet with heightened cardiovascular risk.”
- A “high protein intake is dangerous for people with kidney disease, present in 1 of 7 adults, but 9 of 10 people with reduced kidney function are unaware of it.”
My take (borrowed from Dr. Topol): “The body of evidence about protein does not provide support [for] very high protein intake, certainly not in excess of 1.6 g/kg/day…there is no way to store protein in the body…Resistance training is the principal driver for building muscle mass and strength, not high protein intake.” While this article focuses on adults, the premise is similar in children; though, on a per kilogram basis, children need modestly higher amounts. (Reference: JL Hudson et al. Nutrients. 2021 May 5;13(5):1554. Dietary Protein Requirements in Children: Methods for Consideration)
Related blog posts:
- “Optimal dietary patterns for healthy aging”
- “You Can’t Outrun a Bad Diet”
- NY Times: “Our Food is Killing Too Many of Us”
- Impact of Ultra-Processed Foods on Bowel Health
- The Paramount Health Challenge for Humans in the 21st Century
- Call For Action: Adolescent Nutrition Series | gutsandgrowth
- Ultraprocessed Food and the Risk of Inflammatory Bowel Disease
- Is Red Meat More Likely to Cause High Cholesterol Than White Meat?
- For Increased Longevity: More Greens are Good
- Heart-healthy Mediterranean Diet
- Why Fiber (Fruits and Veggies) is Good for You
- Fresh Fruit Study
- Does a Healthy Lifestyle Result in Better Outcomes?
