N Sengupta et al. Am J Gastroenterol 2024; 119: 438-449. Open Access! The Role of Imaging for Gastrointestinal Bleeding: Consensus Recommendations From the American College of Gastroenterology and Society of Abdominal Radiology. Thanks to Dr. Benjamin Gold for this reference.
This article was jointly published: Radiology 2024; 310(3):e232298
This article focuses on GI bleeding in adults; it has a lot of useful information about the advantages, disadvantages, techniques and performance date of numerous radiology tests which can help sort out GI bleeding.

Some of the recommendations for Overt Lower GI Bleeding:
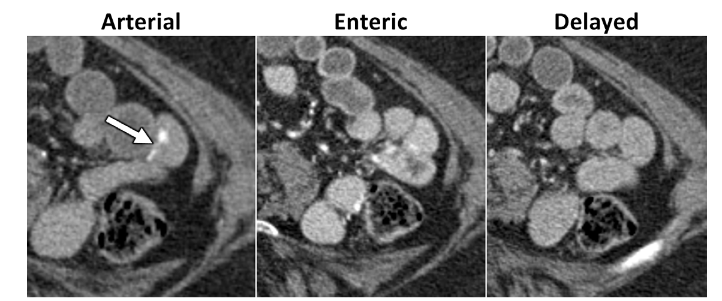
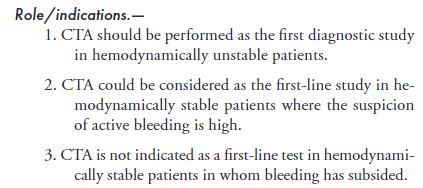
CT Angiography:
Catheter Angiography:

99mTc-RBC Scan

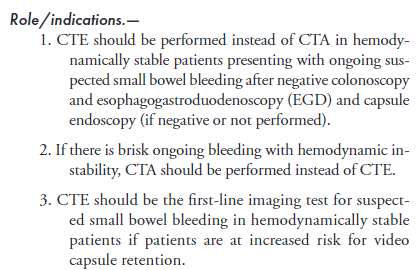
For Suspected Small Bowel Bleeding:
CT Enterography (uses oral contrast). Technique: CTE should be performed using multiphase technique in patients older than 40 years of age where vascular lesions are a common cause for bleeding.
Meckel’s Scan “A Meckel scan can be considered to identify the cause of unexplained intermittent GI bleeding in children and adolescents after negative endoscopic evaluation, including capsule endoscopy if available, and cross-sectional evaluation of the small bowel.”
Radiology compared to capsule endoscopy and balloon-assisted endoscopy The authors discuss the advantages and limitations of radiologic testing versus capsule endoscopy and balloon-assisted endoscopy for small bowel bleeding is provided in Appendix S5
My take: This article provides a good update/review on useful radiologic imaging for GI bleeding. For pediatric GI bleeding, the etiologies are much different and many patients should be evaluated with a Meckel’s scan prior to panendoscopy (depending on the clinical presentation).
Related blog posts:
- Therapeutic Endoscopy Rarely Beneficial in Infants with Gastrointestinal Bleeding
- Meckel’s Scan: “Who are you going to believe, me, or your lying eyes?”
- AAP GI Review Articles: GI Bleeding in the Neonate, Cystic Fibrosis in Neonates, and Intestinal Transplantation in Children
- GI Bleeding -Forrest Classification
- Update on Upper GI Bleeding Recommendations
- Timing of Upper Endoscopy with GI Bleeding -Is It Safer to Wait a Bit?
- Where Did the Blood Go? Case Report
- All Bleeding Stops (part 2)
- All bleeding stops
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.
