A new endoscopic technique’s efficacy has recently been reported (Gastroenterol 2015; 148: 324-33). Since this technique is not likely to be broadly applicable to the pediatric population for some time, I will not delve into all of the details.
In essence, a carefully selected group (n=129 from a screened group of 696) of adult patients with persistent regurgitation underwent transoral fundoplication; this eliminated troublesome regurgitation in 67% compared to 45% who were randomized to sham/PPI. Severe complications were rare.
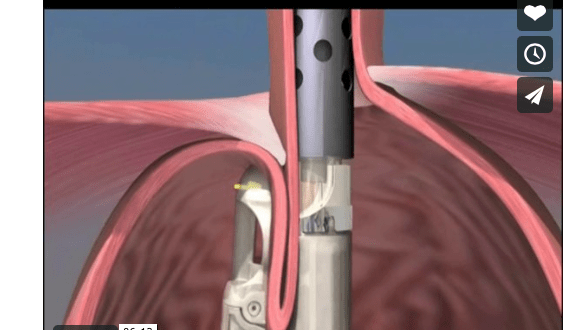
Here is a picture of the technique:
Link: Description and a video animation of the procedure
Bottomline: This endoscopic procedure along with the Stretta procedure and the LINX device (using magnets) offer alternatives to surgical fundoplication in carefully-selected patients with refractory gastroesophageal reflux symptoms.
New drugs approved by FDA:
Ceftolozane (Zerbaxa) -combines a cephalosporin with a beta-lactamase inhibitor (tazobactam). Indications: complicated intra-abdominal infections (in combination with metronidazole), and complicated urinary tract infections. From FDA: FDA approves new antibacterial drug Zerbaxa
Viekira Pak -combination of 3 new drugs: ombitasvir, paritaprevir, and dasabuvir along with older drug: ritonavir. Indications: Hepatitis C genotype 1. From FDA: FDA approves Viekira Pak to treat hepatitis C
Related blog posts to fundoplication: