N Vinit et al. J Pediatr 2022; DOI:https://doi.org/10.1016/j.jpeds.2021.11.004 (Ahead of print) Predicting Factors of Protracted Intestinal Failure in Children with Gastroschisis
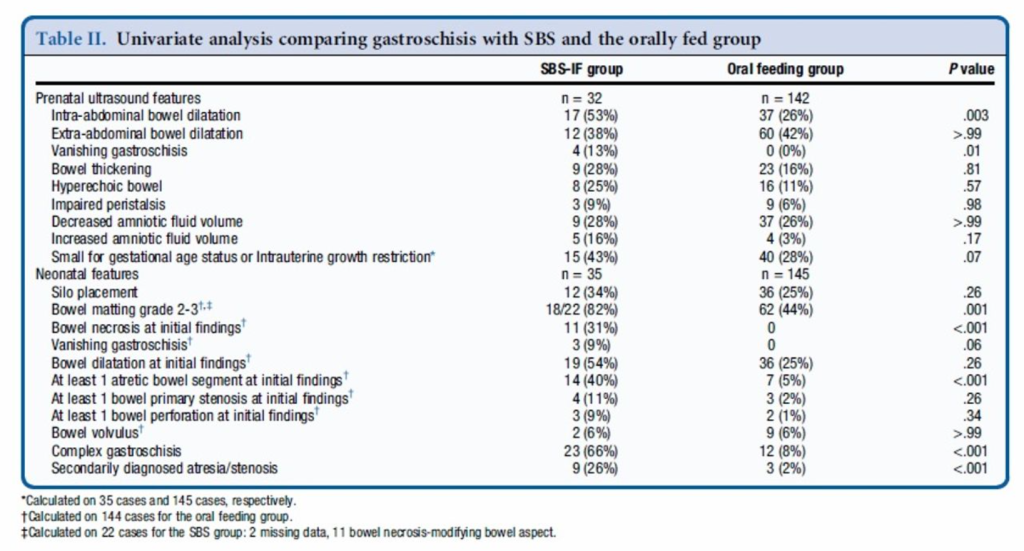
Methods: Retrospective study. Among 180 patients, 35 required long-term parenteral nutrition (SBS-IF group) and 145 acquired full oral feeding within 6 months (oral feeding group) over mean f/u of 7.9 years.
Key findings:
- Both bowel matting (OR, 14.2, P = .039) and secondarily diagnosed atresia or stenosis (OR, 17.78, P = .001) were independent postnatal predictors of SBS-IF.
- An initial residual small bowel length of more than 50 cm was the best predictive cut-off for nutritional autonomy, with a sensitivity of 67% and a specificity of 100%
My take: This study identifies bowel matting and atresia/stenosis as additional factors in predicting nutritional autonomy.
Related blog posts:
- Prospective Outcome Data for Infants with Gastroschisis
- Increasing Rates of Abdominal Wall Defect (Gastroschisis)
- An unexpected finding with gastroschisis management
- Improving Outlook in Neonatal Nutrition (Part 1)
- Enteral Autonomy in Pediatric Intestinal Failure