Dr. Ajay Kaul gave our group a terrific update on chronic intestinal pseudo-obstruction (CIPO). My notes below may contain errors in transcription and in omission. Along with my notes, I have included many of his slides.
Key points:
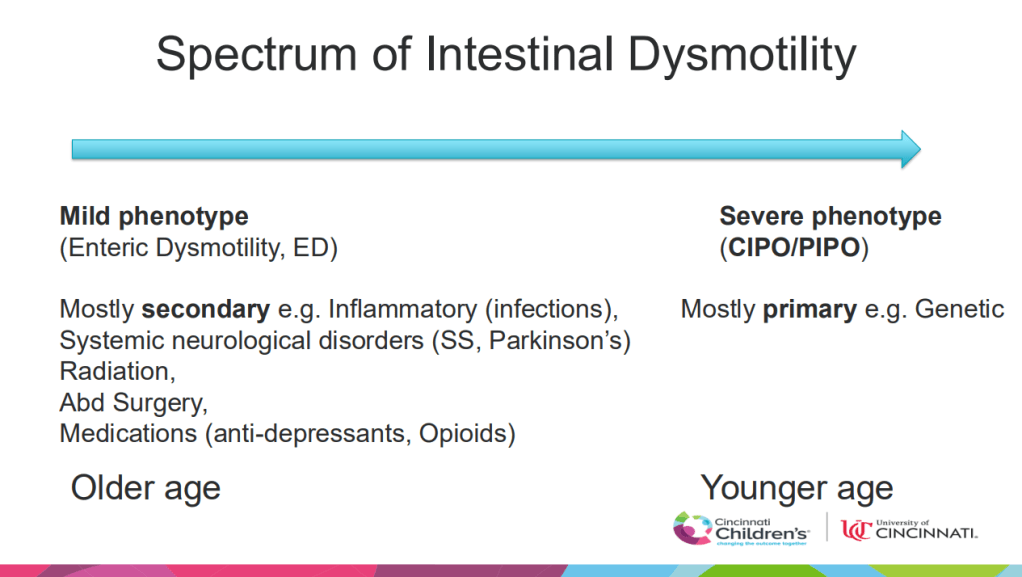
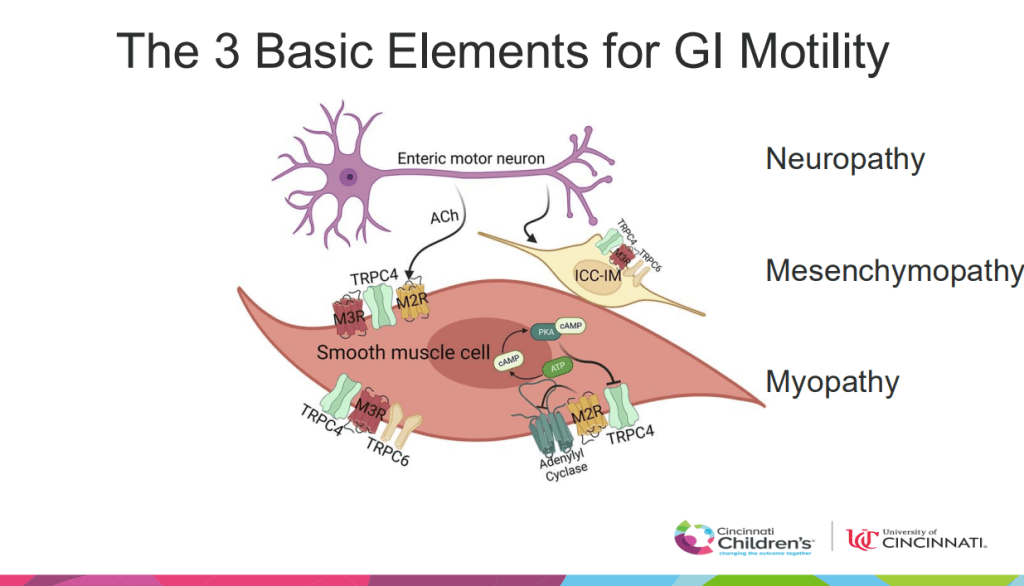
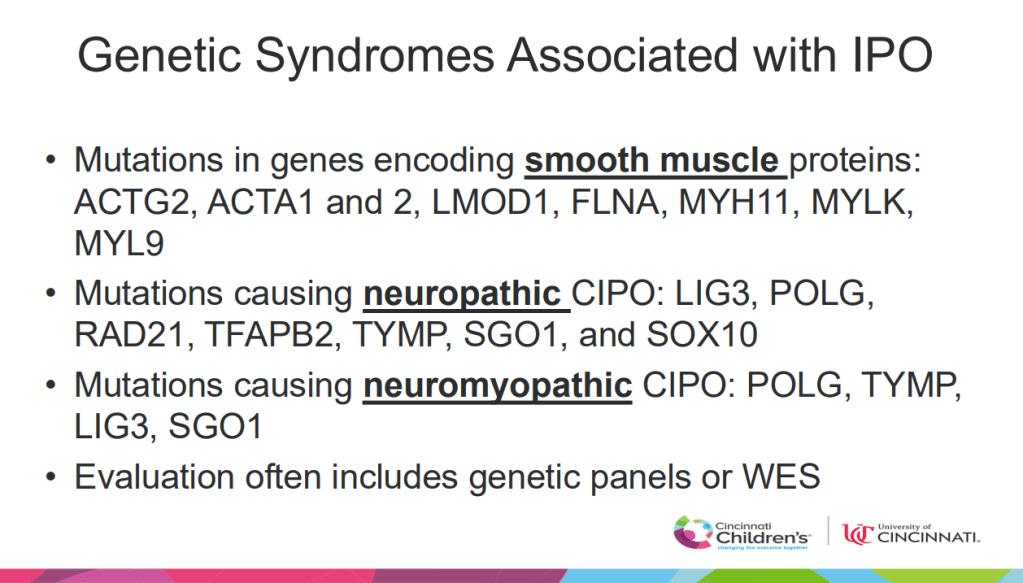
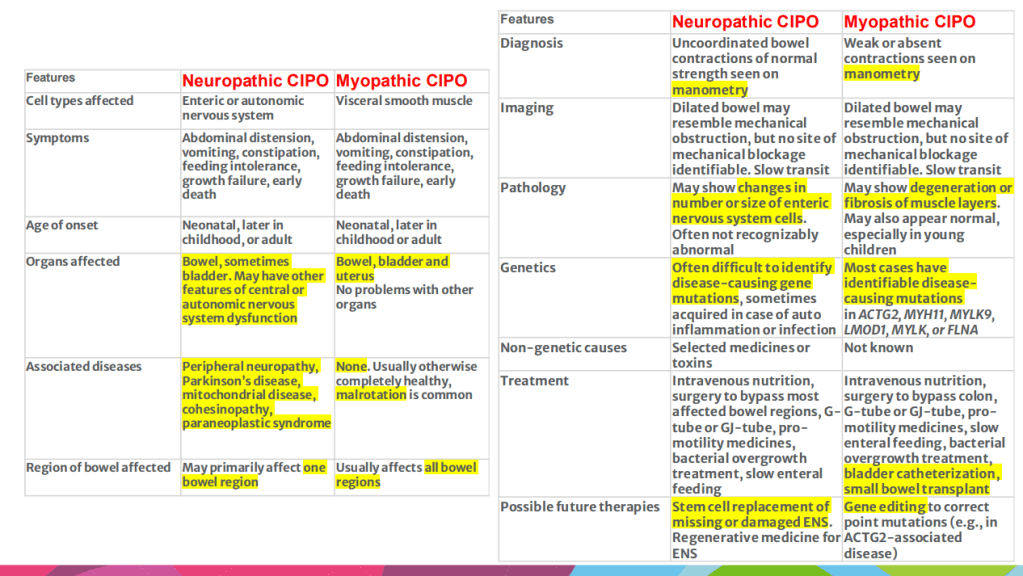
- Several subtypes of intestinal pseudo-obstruction: myopathy, mesenchymopathy, neuropathy
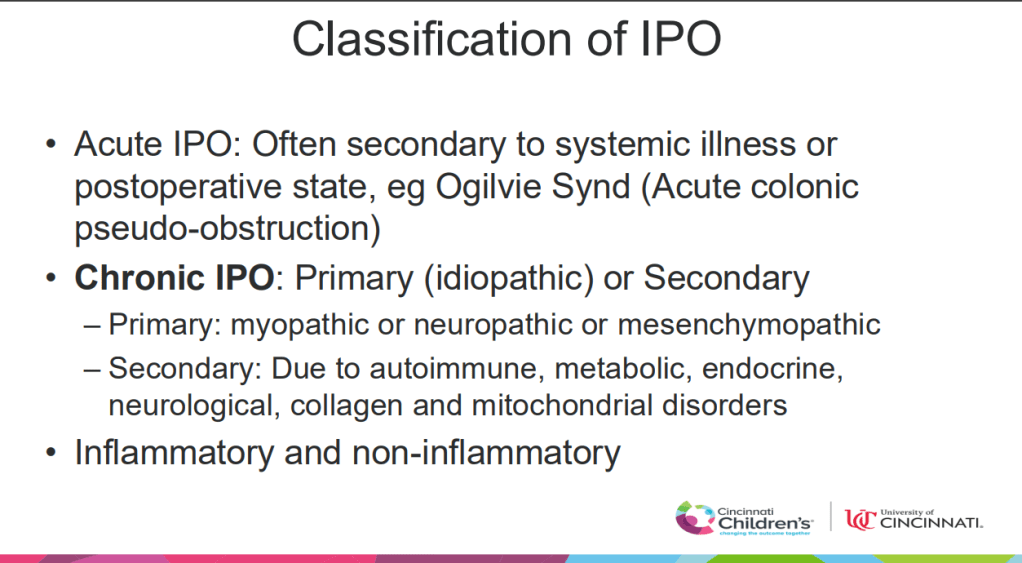
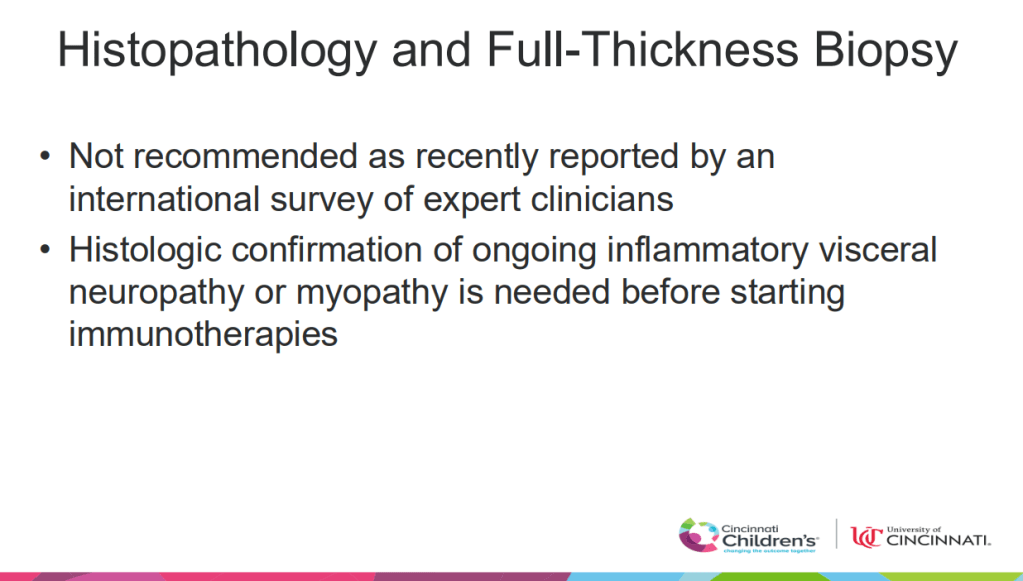
- Also, pseudo-obstruction could be inflammatory versus non-inflammatory. In those with active inflammation, immunosuppression medications may be helpful. However, routine intestinal biopsy is not recommended
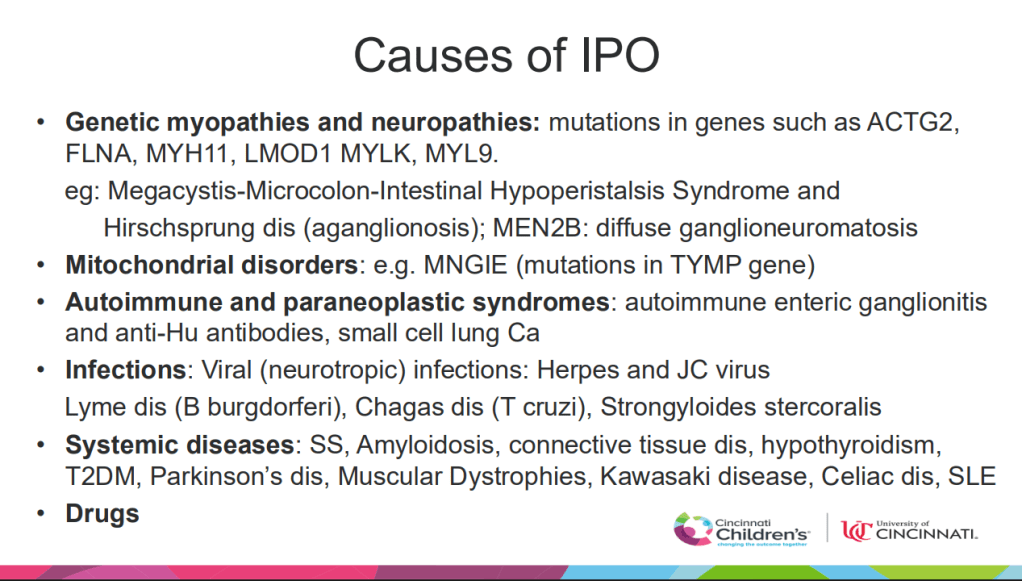
- Gene panel can help with diagnosis
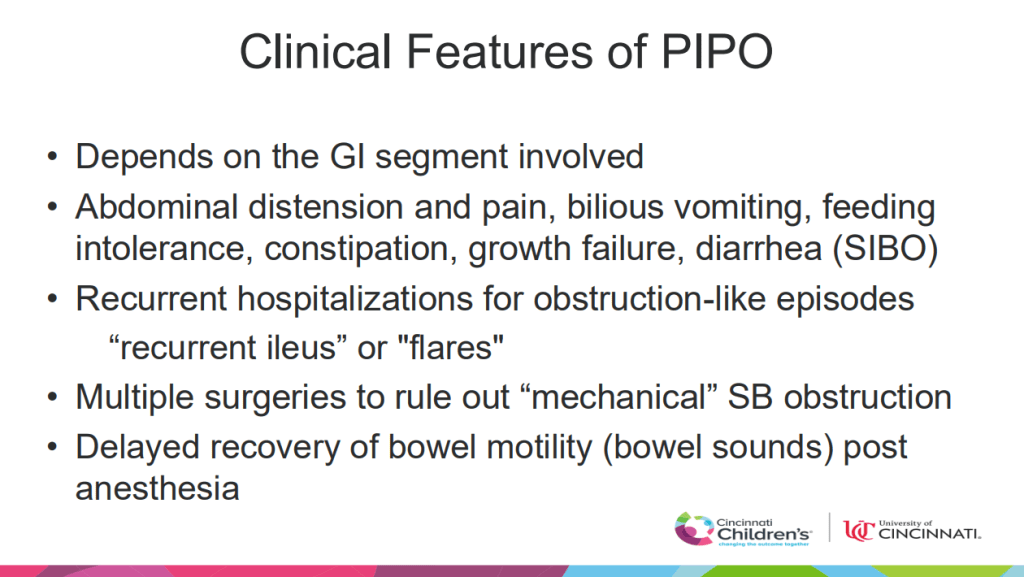
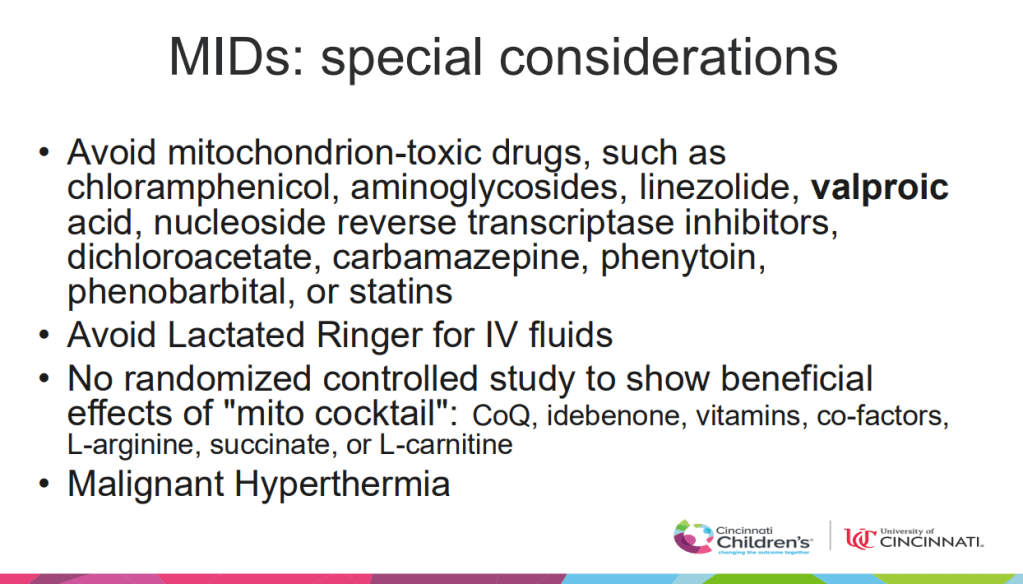
- Anesthesia is associated with delayed recover of bowel function
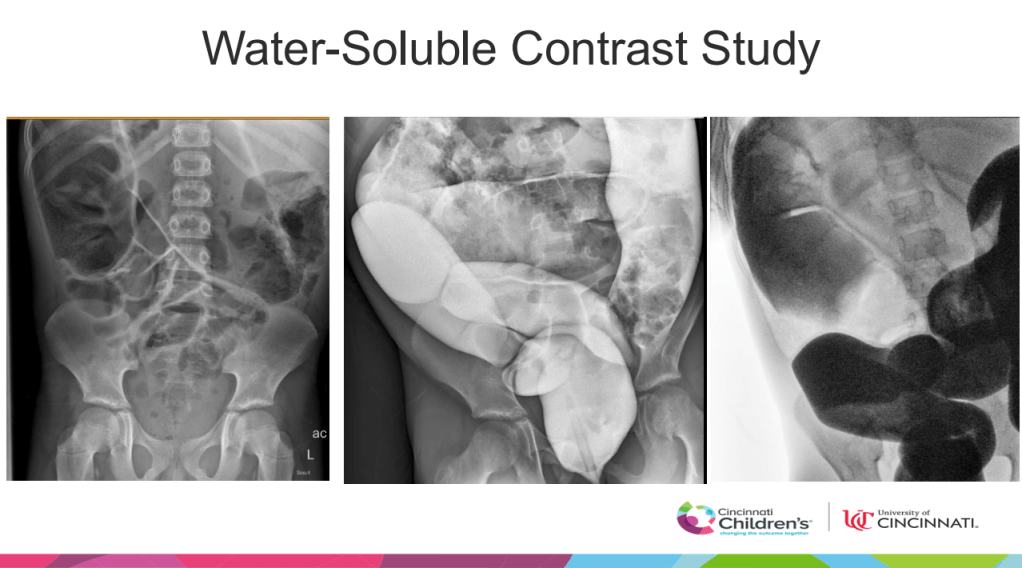
- Malrotaion is associated with myopathic CIPO
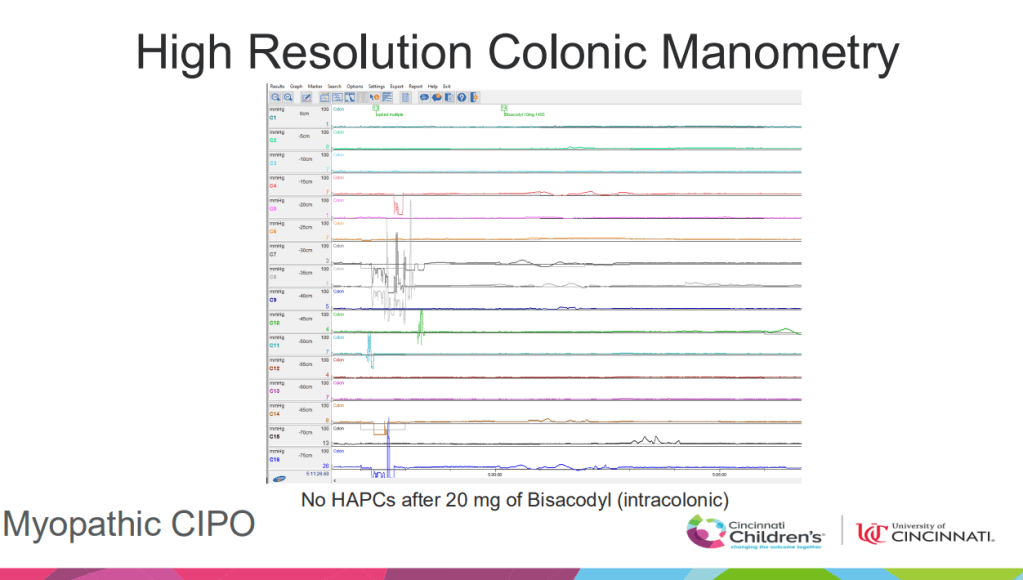
- Myopathic CIPO affects all bowel regions along with bladder/uterus. Myopathic CIPO patients are often good candidates for intestinal transplantation. Neuropathic CIPO can be isolated to one region of the bowel
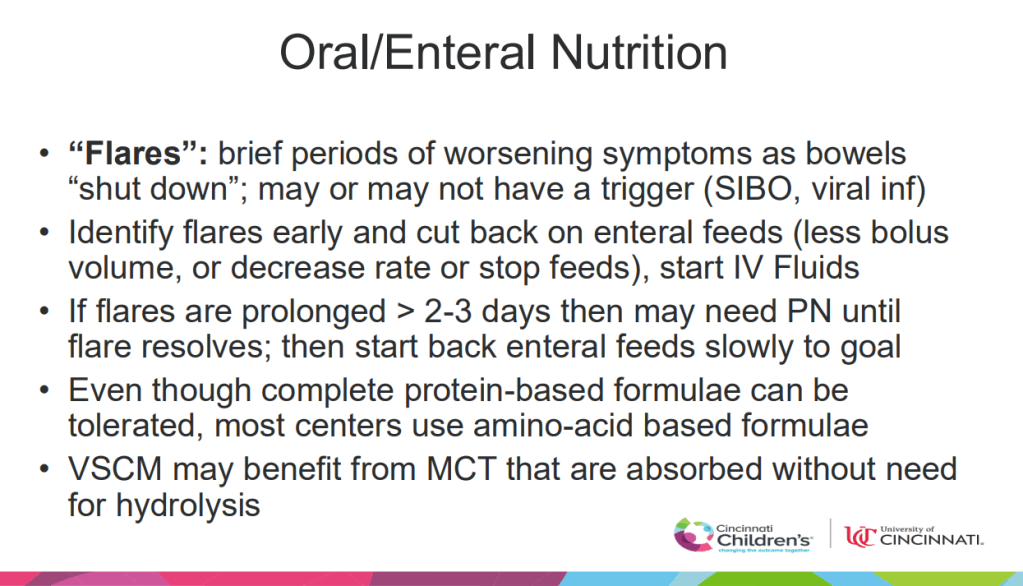
- Flares of CIPO are well-recognized but poorly described. Often, these last for a few days and can be managed with supportive care
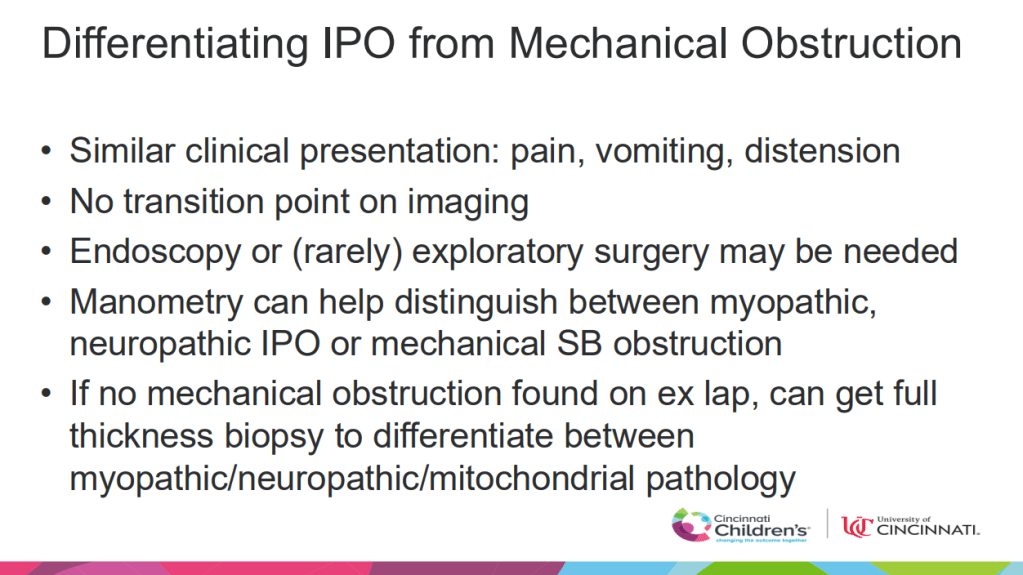
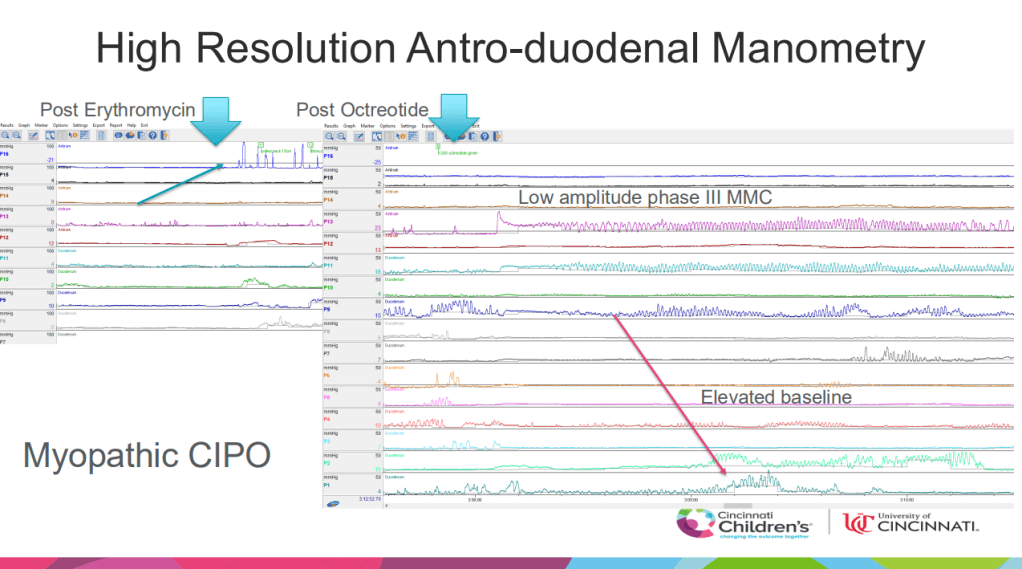
- Myopathic CIPO is characterized by low amplitude phase III MMC on manometry
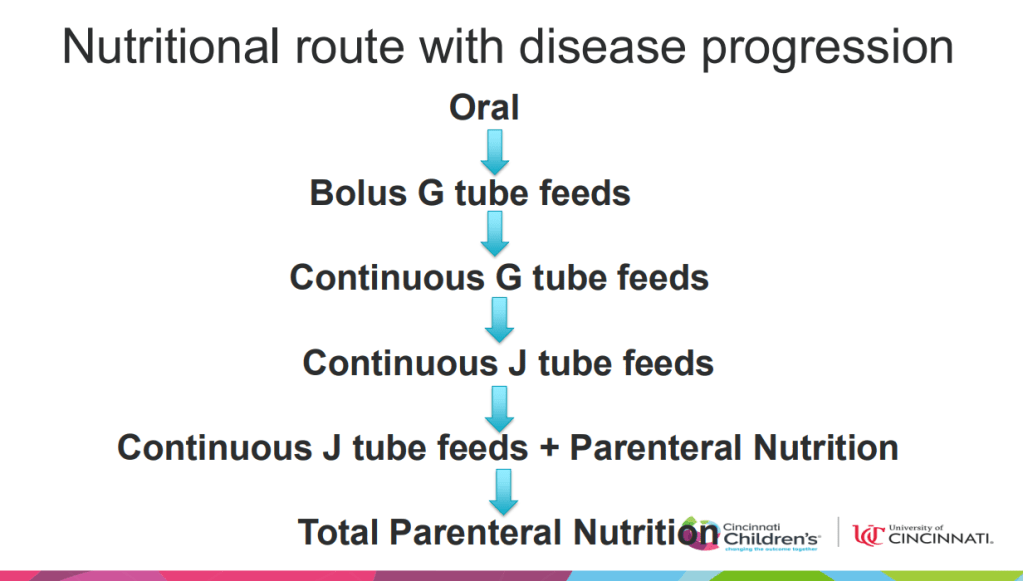
- Monitoring of nutrient deficiencies with CIPO is similar to monitoring for other causes of short bowel syndrome
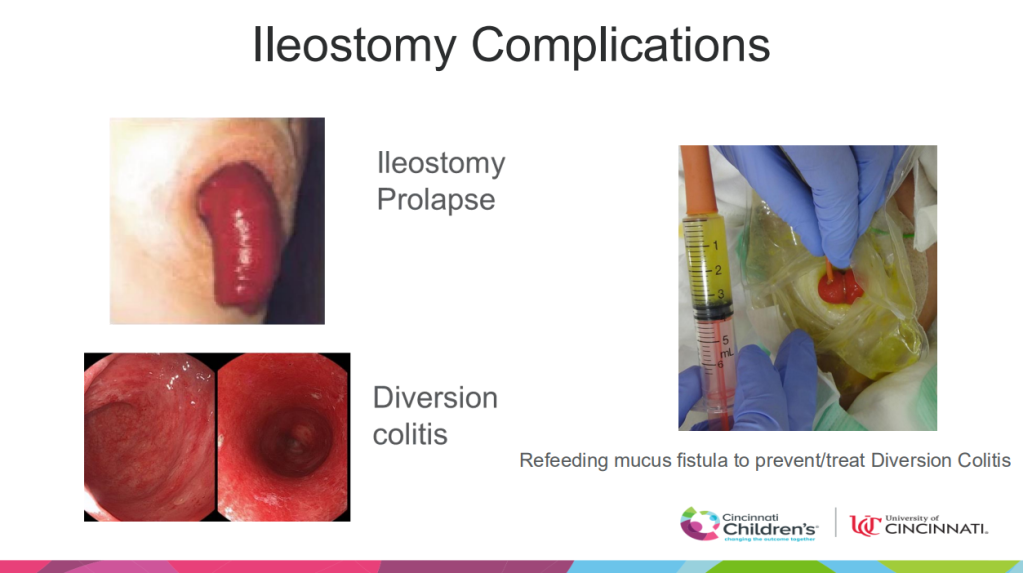
- Ileostomy prolapse and diversion colitis are frequent complications. Diversion colitis can be managed with refeeding into mucus fistula
- Prokinetics are not very effective. Prucalopride may help some. Dr. Kaul often will recommend a 4-week trial and continue if helping. However, prucalopride may contribute to suicidal ideation and families need to be aware of this
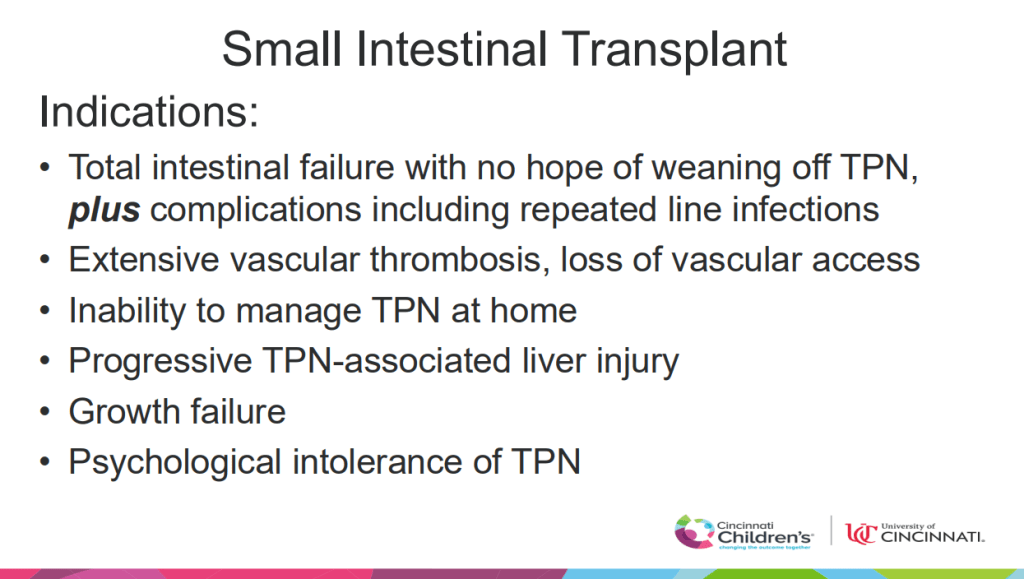
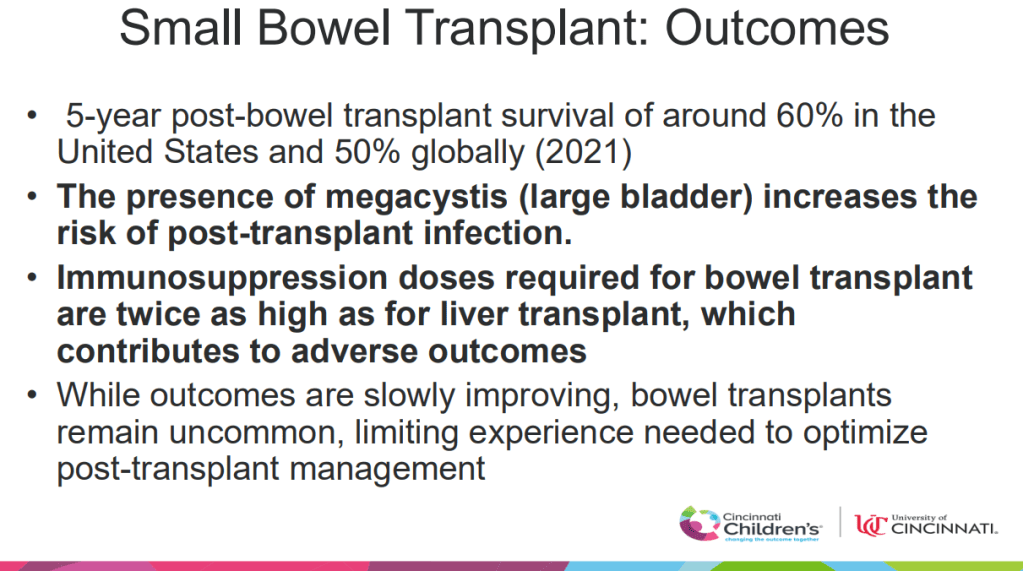
- Intestinal transplantation is being used much less often due to better management of intestinal failure. CCHMC only had one child undergo ITx last year. ITx in U.S. now has an estimated 5-year survival of 60%
- GT placement and ileostomy are frequently needed, especially if trouble tolerating full oral diet
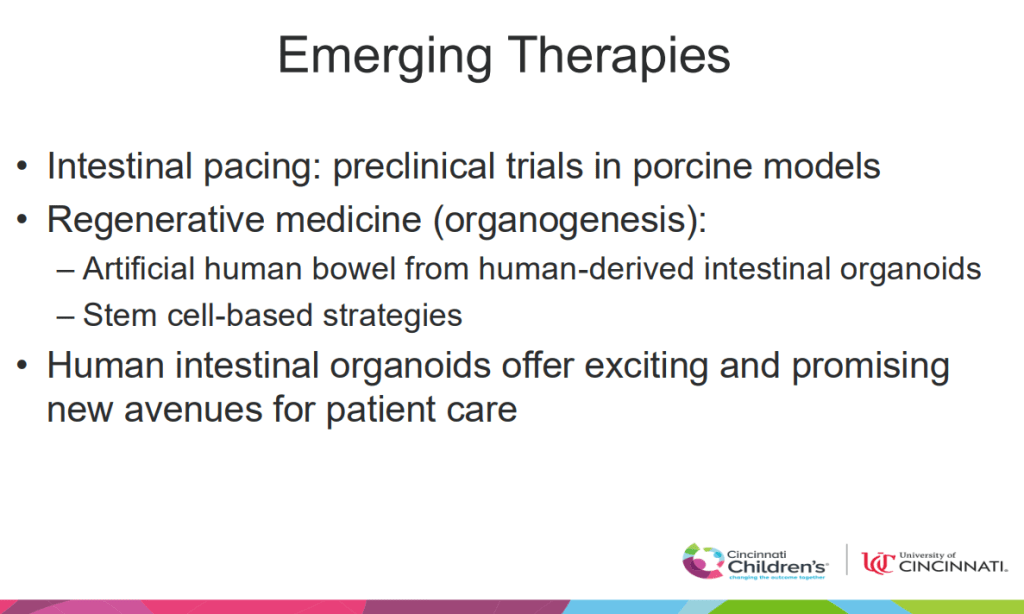
- Several emerging treatments including the use of intestinal organoids are being studied
Related blog posts:






