A Bhattacharjee et al. JPGN 2023; 77: 240-243. Clinical Features of Children With Serology Negative, Biopsy Positive Celiac Disease
At the start of my training in pediatric gastroenterology, the serological testing was not reliable and as a result, very few cases of children who did not have a ‘classical’ phenotype (eg. abdominal distention, poor growth, anemia) were diagnosed. The main exception was the diagnosis in children already recognized as high risk (eg. children with type 1 diabetes).
This recent retrospective study indicates that even with improvement in celiac serology, there are cases of seronegative celiac disease (SN-CD) that are difficult to diagnose. In this study, SN-CD diagnosis required clinical correlation and either confirmatory genetics or follow up endoscopy on a gluten-free diet. Key findings:
- Of the 424 patients who met celiac disease (CD) criteria, 4.7% (n = 20) fulfilled the criteria for SN-CD
- Nearly 65% of SN-CD were IgA sufficient compared with 98.4% in the seropositive group
- All SN-CD patients were symptomatic whereas 82% of seropositive group was symptomatic
The discussion notes that it has been understood that the sensitivity of TTG IgA is about 95% and specificity about 96%. However, the authors caution that this may be “largely overestimated due to failure to account for verification bias. Only 3.6% of IgA-ATTG negative individuals were referred for biopsy” in Hujoel et al meta-analysis (J Clin Gastroenterol 2021; 55: 327-334); thus, the sensitivity could be as low as 57% based on this meta-analysis. In addition, gluten restriction prior to serological testing can further reduce the sensitivity of serological tests.
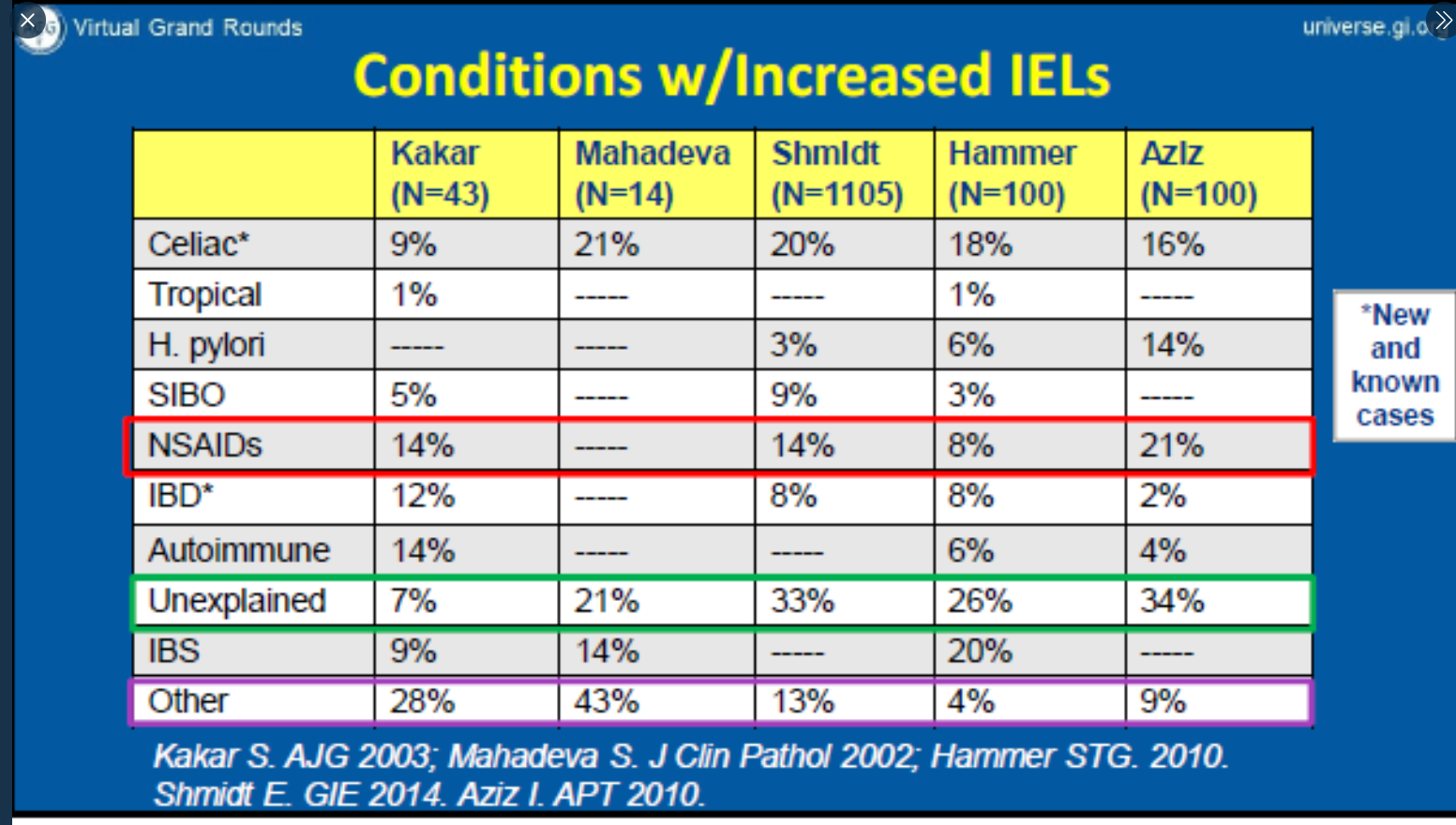
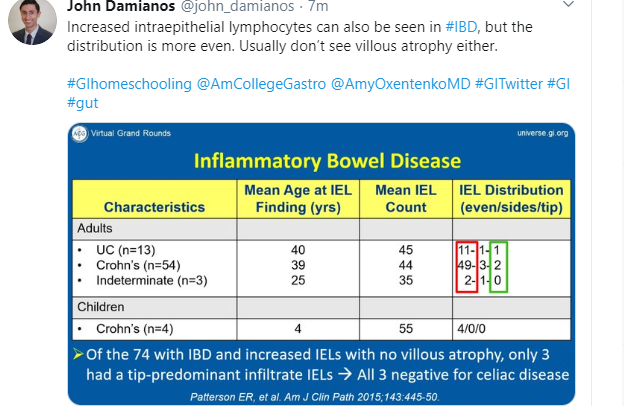
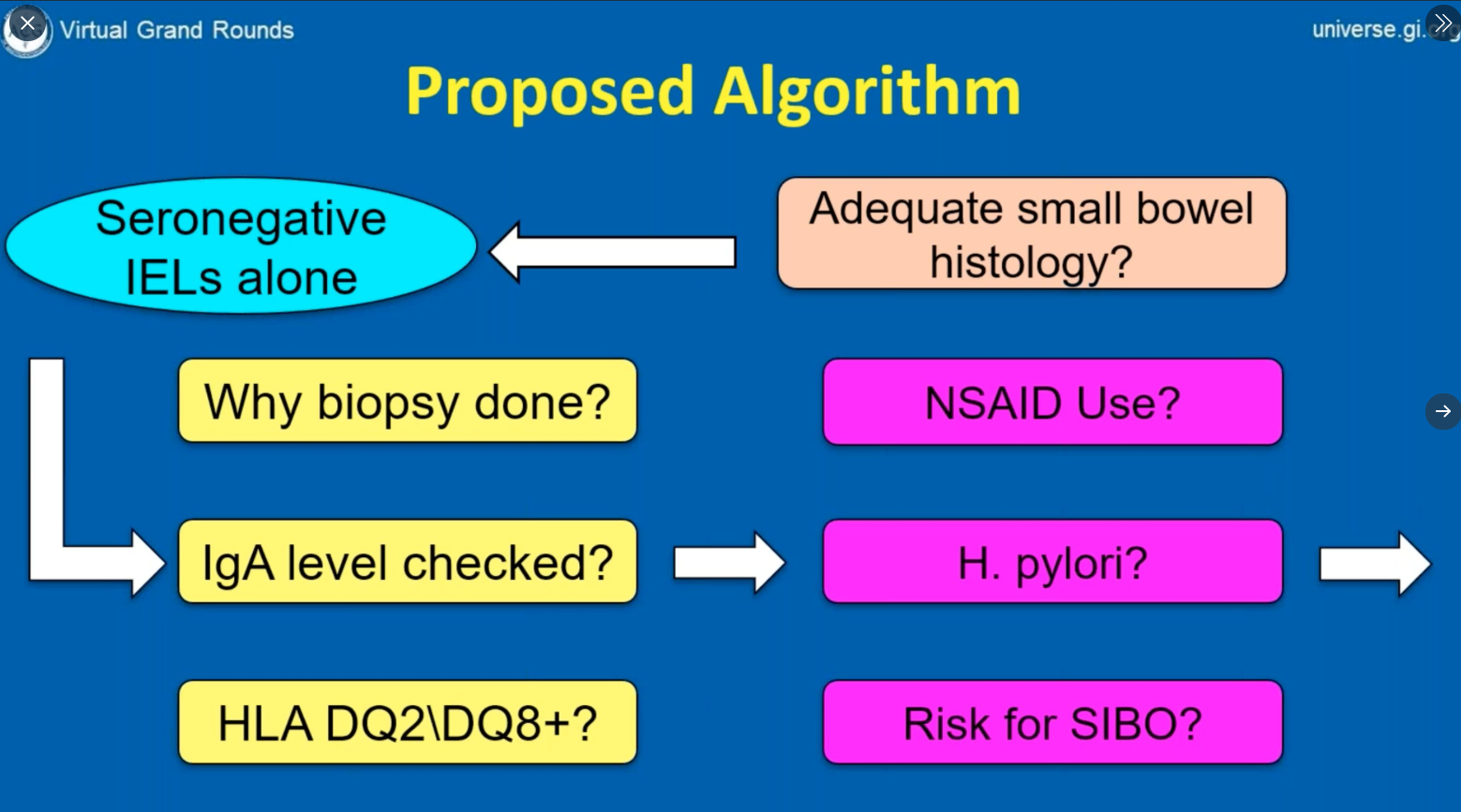
An important limitation of the study is proving that SN-CD was in fact SN-CD and not one of the mimics for CD (eg. inflammatory bowel disease, autoimmune disorders, medication effect). However, they noted that their cohort had followup over 6-9 years and with symptom resolution with a gluten free diet.
My take: Identifying SN-CD is difficult since so many children have similar digestive symptoms unrelated to celiac disease. Most children with vague digestive complaints do not need to undergo endoscopy; as such, SN-CD can be easily overlooked.
Related blog posts:
- @AmyOxentenkoMD: Celiac Disease and Mimics
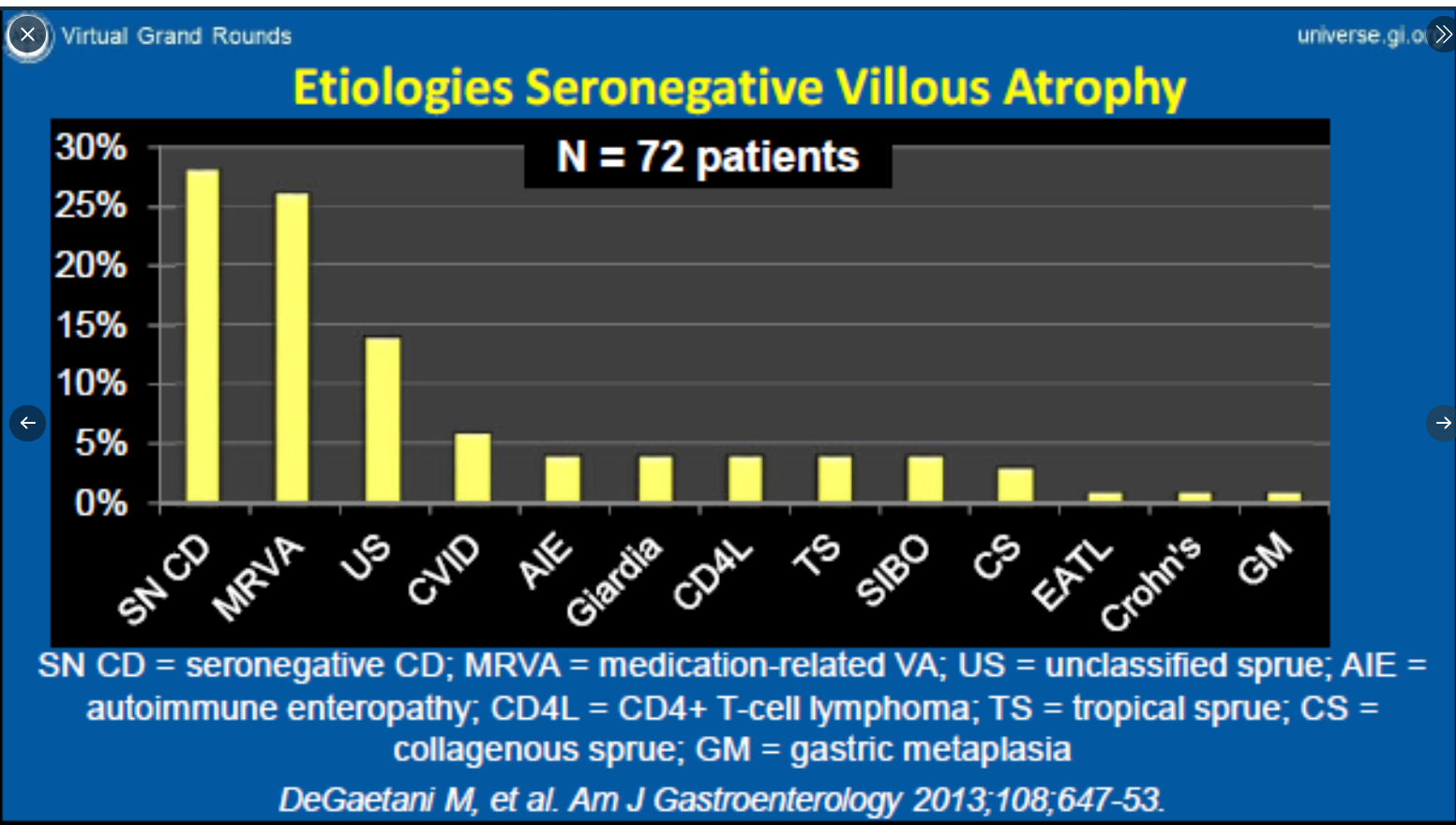
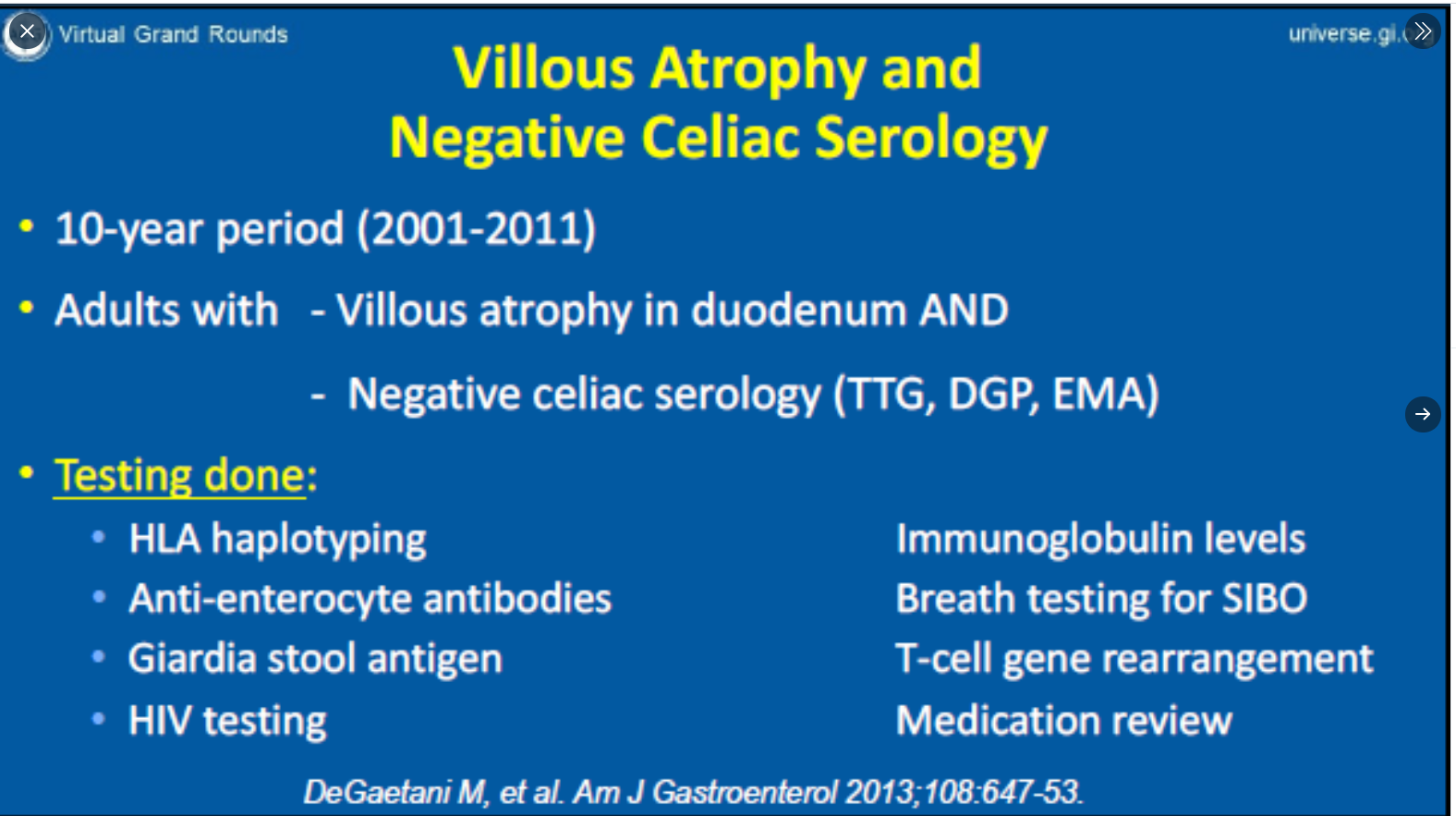
- Seronegative Villous Atrophy
- 2023 ACG Celiac Guidelines for Adult and Children
- Double Whammy: Coexistent IBD and Celiac Disease in Children