A Kruegger et al. JPGN 2025; 81:596–605. Open Access! The prevalence and predictive factors of overlapping disorders of gut–brain interaction and celiac disease in children
Methods: Single-center, retrospective study of children (4–21 years old, n=191) with biopsy-proven Celiac disease (CeD) who were evaluated for DGBI based on Rome IV criteria. Patients who were adherent to a GFD, demonstrated tissue transglutaminase immunoglobulin A (TTG IgA) decline, and had at least one visit 9–24-months after diagnosis with a pediatric gastroenterologist. For this study, sustained TTG IgA decline required at least two declining TTG IgA values, a 90% decline from baseline, or normalization of TTG IgA.
Key findings:
- 43% (n = 83) met Rome IV DGBI diagnostic criteria.
- Functional constipation (27/83, 33%) and functional abdominal pain (24/83, 29%) were the most common DGBI
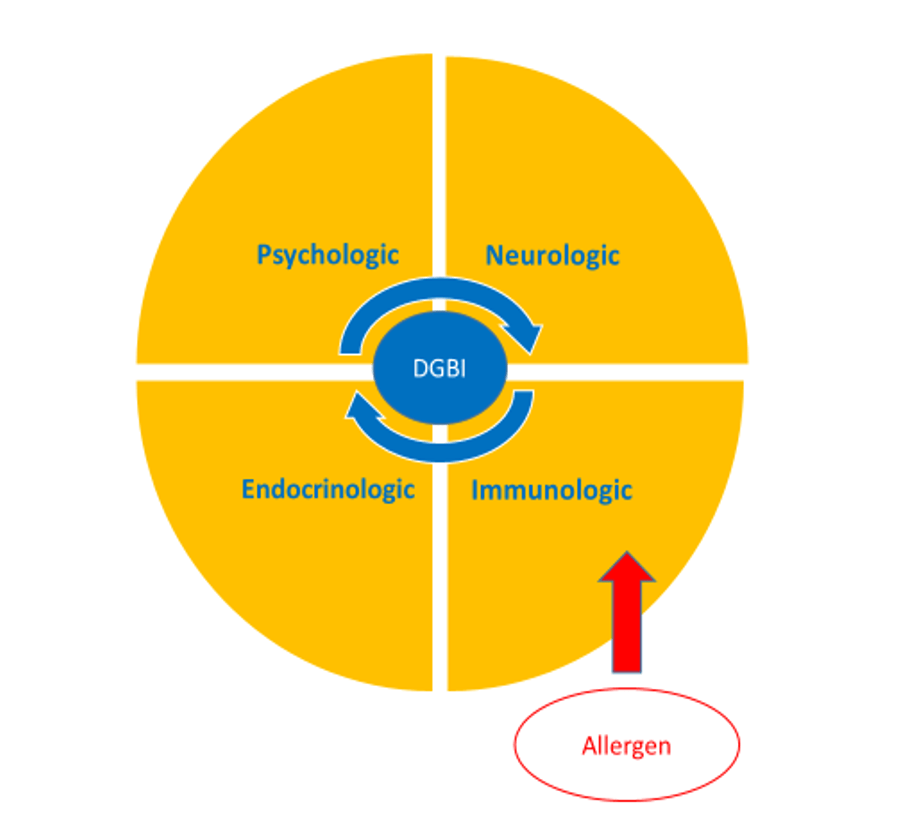
- Abdominal pain, constipation, and vomiting at initial presentation as well as comorbid joint hypermobility, headaches, and chronic musculoskeletal pain increased risk of developing DGBI after serological decline
Discussion Points:
- “The prevalence reported here is similar to a study of adults with CeD who were adherent to a GFD that reported over 50% met criteria for a functional gastrointestinal disorder19 and is higher than previously reported pediatric prevalence rates”
- “The majority of patients who met DGBI criteria did so through having the persistence of the same gastrointestinal symptoms that were present at CeD diagnosis. This raises the question as to whether the symptoms at presentation were due to CeD, DGBI, or both”
- “Clinicians could consider discussing that while symptoms related to CeD should improve on a GFD, some symptoms may persist, especially if they have an increased likelihood of having a comorbid DGBI. Such counseling may prevent the misattribution of persistent symptoms to ongoing gluten exposure and mitigate hypervigilance”
- “Having complete villous blunting on diagnostic biopsy increased the likelihood of having a DGBI. Intuitively, it is possible that complete villous blunting can lead to greater nerve sensitization and subsequently higher rates of DGBI. It is also possible that complete villous blunting is slower to recover”
My take: Given the overlap of DGBI symptoms with CeD, diagnosing DGBI in patients with CeD can be challenging. However, DGBI is much more likely to contribute to lingering symptoms than refractory CeD.
As a practical matter, the high frequency of ongoing GI symptoms despite use of a GFD provides another drawback to relying on a no-biopsy diagnosis. A no-biopsy diagnosis introduces greater uncertainty in the diagnosis and does not allow for a histologic comparison if a subsequent evaluation is needed.
Related blog posts:
- New Data on the Reliability of the No-Biopsy Diagnosis in Pediatric Celiac Disease
- Increased Risk of Irritable Bowel Before and After the Diagnosis of Celiac Disease
- Treatment of Refractory Celiac Symptoms with a Low FODMAP Diet
- What To Do For Pediatric Patients with Non-Responsive Celiac Disease
- Persistent Villous Atrophy in Celiac Disease Despite a Gluten-Free Diet
- Functional Abdominal Pain in Children with Celiac Disease
- Dr. Arun Singh: Tips and Tricks to Managing Celiac Disease
- How to Diagnose Celiac Disease in Patients Already Receiving a Gluten Free Diet
- Work Disability with Celiac Disease
- Dr. Neha Santucci: Management of DGBIs in the Post-Pandemic Era (Part 1)
- Real-World = Partially-Treated Celiac Disease
- Celiac Disease: “”80 percent of success is just showing up”
- Is a Gluten-Free Diet Possible? DOGGIE BAG Study
- How Slow Do Objective Markers of Celiac Disease Improve
- How Accurate is Serology at Predicting Mucosal Healing in Pediatric Patients with Celiac Disease