I recently had the opportunity to hear a terrific lecture by David Adamkin (University of Louisville) on neonatal nutrition. Unlike previous lectures that I’ve highlighted on this blog (Neonatal Nutrition Lecture -What We Know Right Now …) which focused on enteral nutrition and breastmilk. This lecture focused on providing early parenteral nutrition to prevent postnatal growth failure.
Introduction of TPN dramatically improved survival for many infants. In disorders like gastroschisis, TPN increased survival from ~10% to 90%.
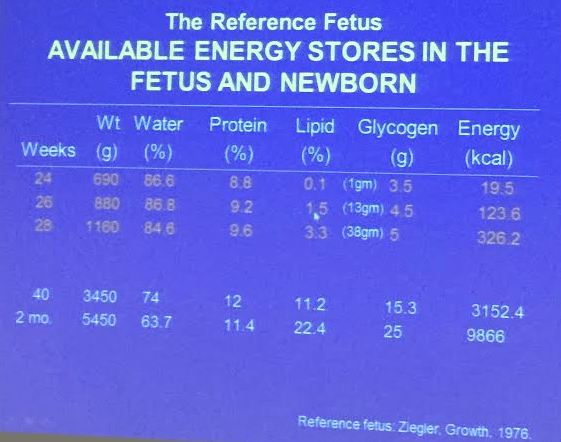
At 24-28 weeks gestational age, fetuses are ‘bathed in amino acids’ and extreme premature infants need early amino acids. At University of Louisville, the neonatologists try to deliver ~3 gm/kg/day of amino acids in 1st 1-2 days in order to match intrauterine growth and prevent growth failure. Half of postnatal weight loss is water; other half is related to proteolysis. To facilitate TPN at all hours, they use a stock solution (4% amino acids at 60 mL/kg/day delivers 2.4 mg/kg/day of protein; 80 mL/kg/day delivers 3.2 mg/kg/day of protein.

Return to Birth Weight Time is Correlated with Growth Failure. Extreme prematurity has been correlated with slower return to birth weight
BUN increases with any protein intake but not affected by protein intake -issue has to do renal fxn, comorbidity. Smaller & sicker have higher BUN.
Key points:
- The more premature, then the longer it takes to return birth weight and more growth failure
- Poor growth related to neurodevelopment outcomes
- With higher protein intake, there is better glucose tolerance; protein intake helps with glucose tolerance & lowers chance of hyperkalemia
More tomorrow…