D Cook et al. NEJM 2024; 391: 9-20. Stress Ulcer Prophylaxis during Invasive Mechanical Ventilation
This international, randomized trial assigned critically ill adults (n=4821) who were undergoing invasive ventilation to receive intravenous pantoprazole (at a dose of 40 mg daily) or matching placebo. Both groups included ~22% who had had PPIs prior to hospitalization. The primary efficacy outcome was clinically important upper gastrointestinal bleeding, identified locally as overt gastrointestinal bleeding with evidence of hemodynamic compromise or leading to therapeutic interventions in the ICU (or resulted in readmission to the ICU during the index hospital stay) up to 90 days after randomization.
Key findings:
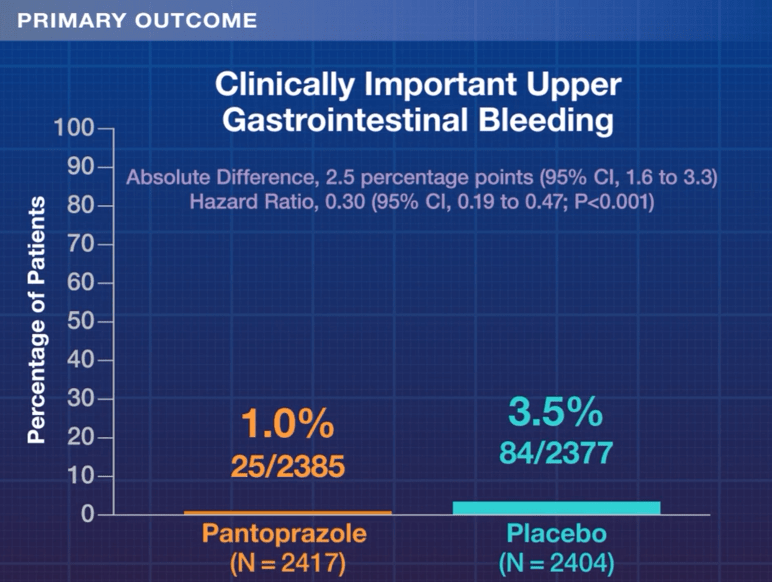
- Clinically important upper gastrointestinal bleeding occurred in 25 of 2385 patients (1.0%) receiving pantoprazole and in 84 of 2377 patients (3.5%) receiving placebo (hazard ratio, 0.30; P<0.001)
- At 90 days, death was reported in 696 of 2390 patients (29.1%) in the pantoprazole group and in 734 of 2379 patients (30.9%) in the placebo group (hazard ratio, 0.94; P=0.25)
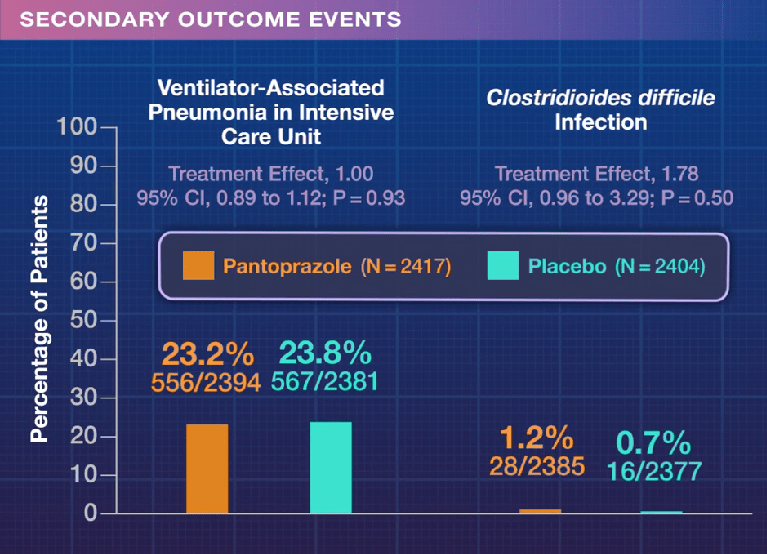
- PPI-treated patients had similar rates of ventilator-associated pneumonia and C diff infection

In the associated editorial, (SM Brown. NEJM 2024; 391: 78-79) noted that “two previous trials, SUP-ICU1 and the cluster-randomized PEPTIC2 (which compared proton-pump inhibitors with placebo and H2-receptor blockade, respectively), suggested that the effects on mortality may differ according to patients’ disease severity — and that the drugs were potentially less safe in more severely ill patients.”
“Proton-pump inhibitors slightly but significantly decrease the risk of important gastrointestinal bleeding and have a decent chance of slightly decreasing mortality in less severely ill patients during mechanical ventilation. Moreover, we can be certain that proton-pump inhibitors do not decrease — and may slightly increase — mortality in severely ill patients…For sicker patients, I would probably reserve the use of proton-pump inhibitors for those who are being treated with antiplatelet agents, especially in the presence of therapeutic anticoagulants.”
My take: This study and editorial helps provides insight into the narrow path of benefit that PPIs may provide for ventilated adults in the ICU. This study reinforces my view that there are few circumstances where adding empiric PPIs in children would be beneficial. Children are less likely to have significant GI bleeding than adults and have fewer comorbidities. Thus, PPIs in pediatrics need to be used mainly in the context of active GI bleeding and in children needing treatment for specific etiologies. PPIs have low value in most children as prophylaxis (e.g. children with IBD receiving steroids).
Related blog posts:
- All Bleeding Stops (part 2)
- Is PPI Use Detrimental Before or After a Diagnosis of Inflammatory Bowel Disease?
- Do PPIs Increase the Risk of Eosinophilic Esophagitis in Patients with Esophageal Atresia?
- Austin Bradford Hill, PPIs and IBD
- Positioning Radiology Tests for GI Bleeding
- Understanding Protopathic Bias and Safety of Proton Pump Inhibitors & COVID-19 Worldwide Nadir
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.

