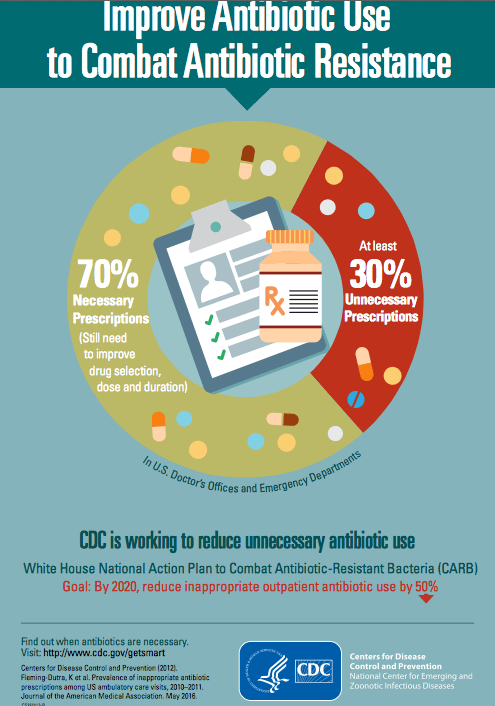
A recent study by Fleming-Dutra K et al (JAMA, May 2016), that has been widely reported, estimates that 1 in 3 antibiotic prescriptions in U.S. are unnecessary. Here’s a CDC media release link: CDC: 1 in 3 antibiotic prescriptions unnecessary
“About 44 percent of outpatient antibiotic prescriptions are written to treat patients with acute respiratory conditions, such as sinus infections, middle ear infections, pharyngitis, viral upper respiratory infections (i.e., the common cold), bronchitis, bronchiolitis, asthma, allergies, influenza, and pneumonia. An estimated half of these outpatient prescriptions are unnecessary.”
Some of the downside of unnecessary antibiotics:
- Allergic reactions and other adverse reactions
- Infections become more difficult to treat due to increased resistance
- Expense
- Clostridium difficile infection
My take: This study’s findings are NOT surprising. Antibiotics are often prescribed without a clear indication.
Many children are labelled allergic to antibiotics like amoxicillin due to the development of a rash but have not undergone formal evaluation. However, a recent study (Mill C et al. JAMA Pediatr 2016 Apr 4) shows that an oral provocative challenge that most will be able to tolerate amoxicillin. Here is a summary of the article by DocAlert (forwarded to me by Mike Hart) -I highlighted in bold the key finding:
In an observational study, researchers offered a graded oral provocation test to all children referred to an allergy clinic in Montreal with suspected allergy to amoxicillin. Children were given 10% of the therapeutic dose of amoxicillin, observed for 20 minutes, then given 90% of the therapeutic dose and observed for at least 1 hour. Parents were instructed to report reactions that occurred the next week.
Of 818 participants (mean age, 1.7 years), 94% tolerated the provocation test and therefore were not allergic to amoxicillin. Of the others, 2% had immediate reactions (within 1 hour of the last dose) — all mild urticaria that resolved with antihistamines — and 4% had nonimmediate reactions (median of 12 hours after the last dose) — all mild maculopapular rash. Only 1 of the 17 children with immediate reactions tested positive on skin prick and intradermal testing 2 to 3 months later.
History of a rash lasting longer than 7 days and parental history of drug allergy were associated with nonimmediate reactions on the provocation test (adjusted odds ratios, 5 and 3, respectively); history of allergic reaction within 5 minutes was associated with immediate reactions (AOR, 10). During 3-year follow-up of children who tolerated the test, 55 received a subsequent full course of amoxicillin and 6 (11%) had nonimmediate reactions. All patients with reactions to amoxicillin tolerated cefixime.
My take (from summary): An oral provocation challenge to confirm either an immediate or nonimmediate allergic reaction to amoxicillin was found to be safe and more accurate than skin testing.