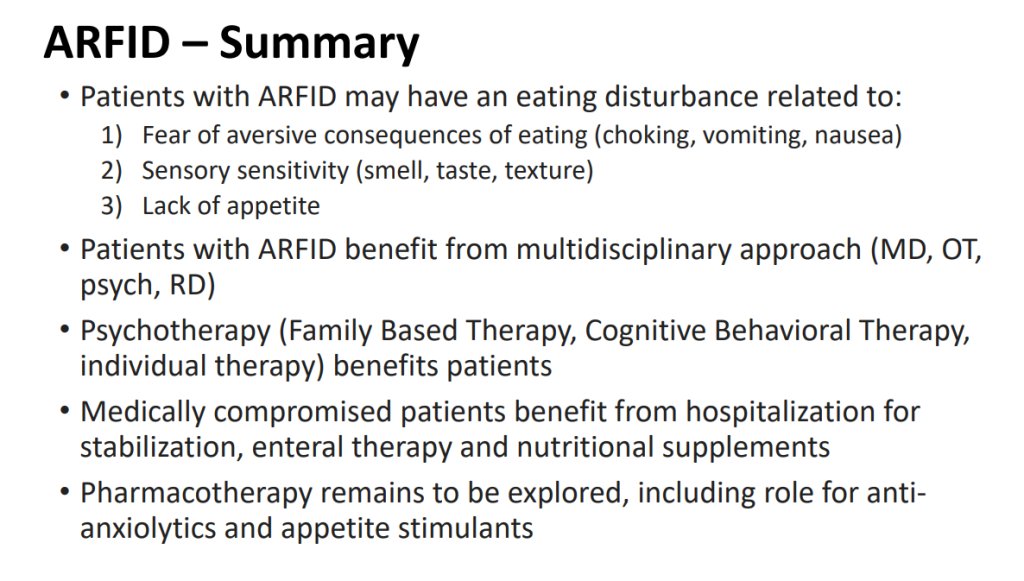
Recently, at the Georgia AAP Pediatrics by the Sea meeting, Mel Heyman presented a terrific lecture reviewing ARFID. This lecture delved into the historical backgrounds of eating disorders and described the subtypes of ARFID along with evaluation/management. This lecture was presented in honor of Stan Cohen who recently retired from our group. Here are many of the slides:













Related blog posts:
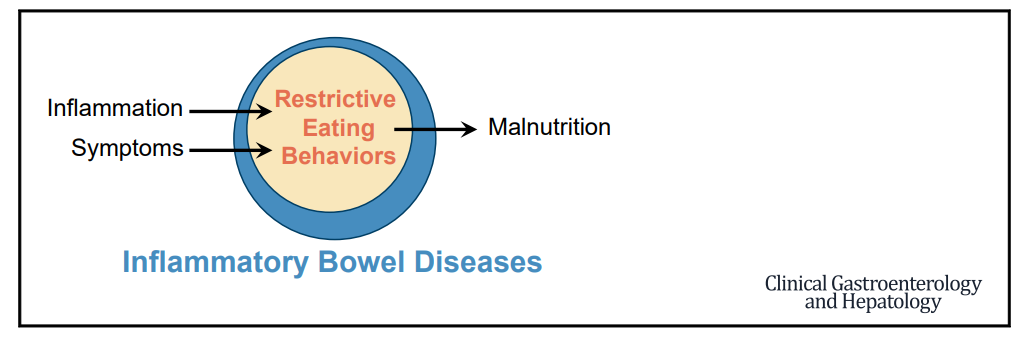
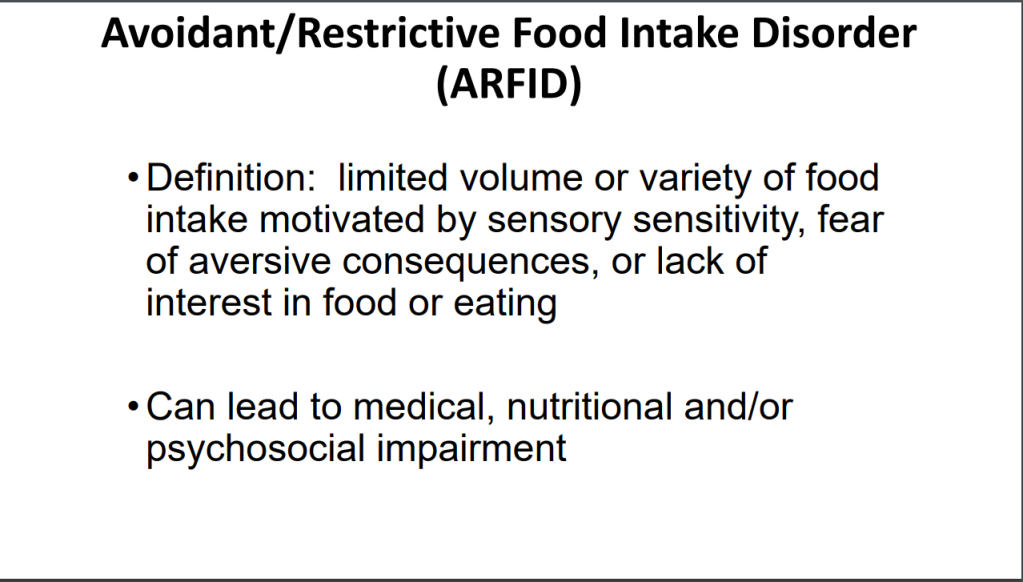
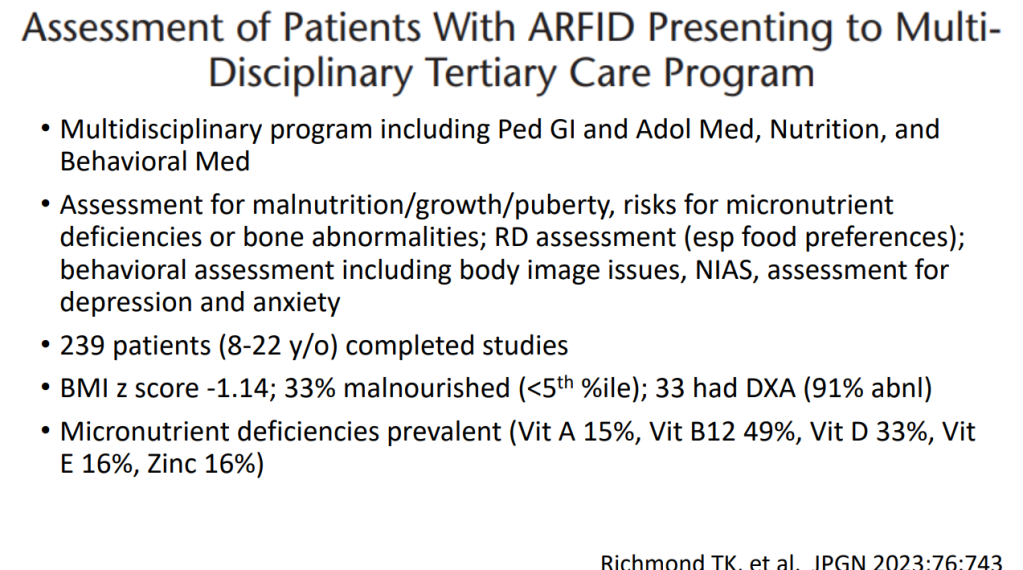
- Avoidant/Restrictive Food Intake Disorder (ARFID) with Irritable Bowel Syndrome and with Inflammatory Bowel Disease
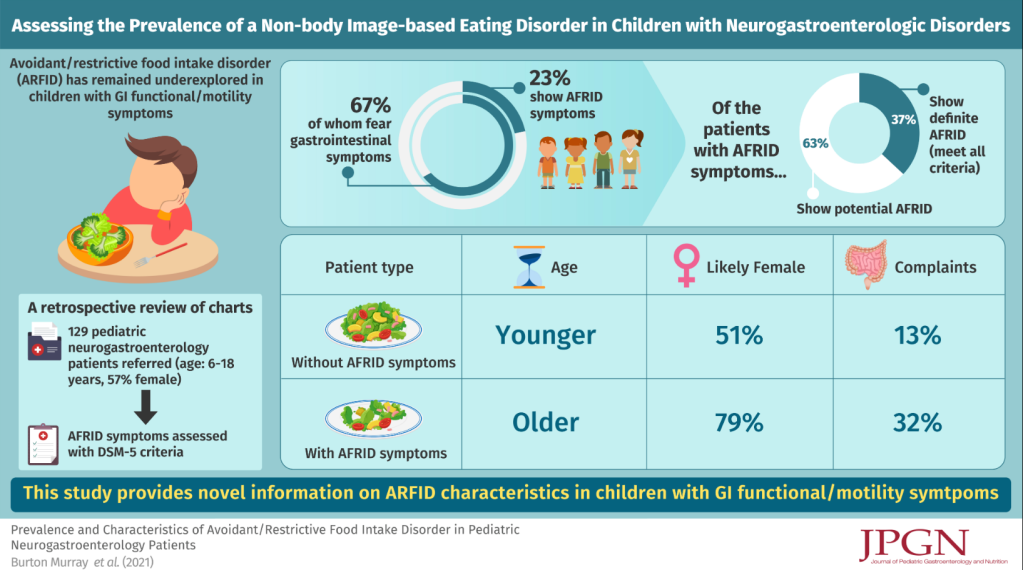
- Prevalence of Avoidant/Restrictive Food Intake Disorders in Pediatric Neurogastroenterology
- Afraid to Eat -Could be “Avoidant Restrictive Food Intake Disorder”
- Picky Eating and Underlying Psychological Problems
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.