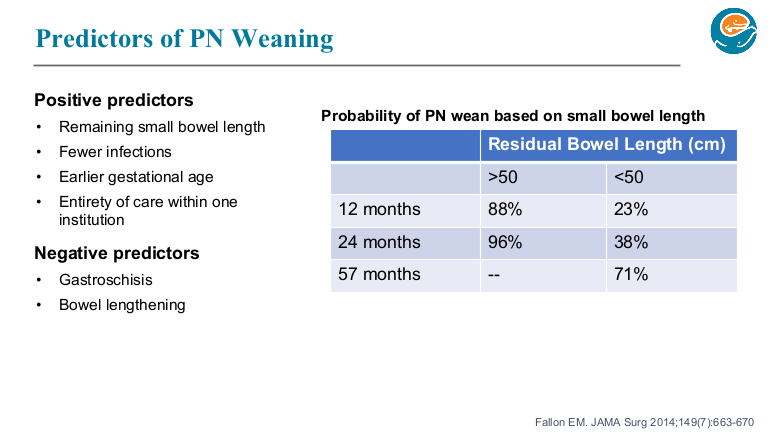
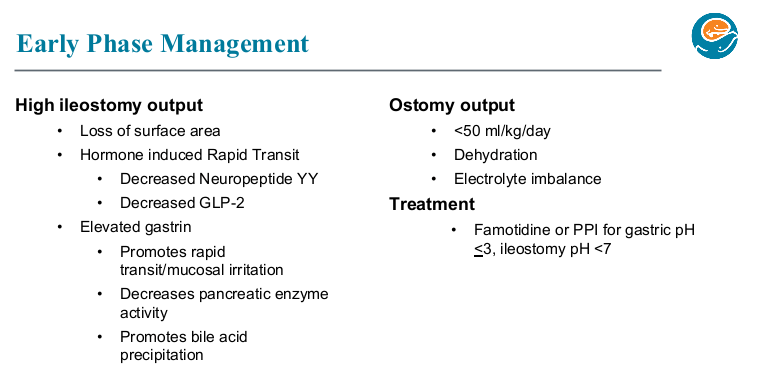
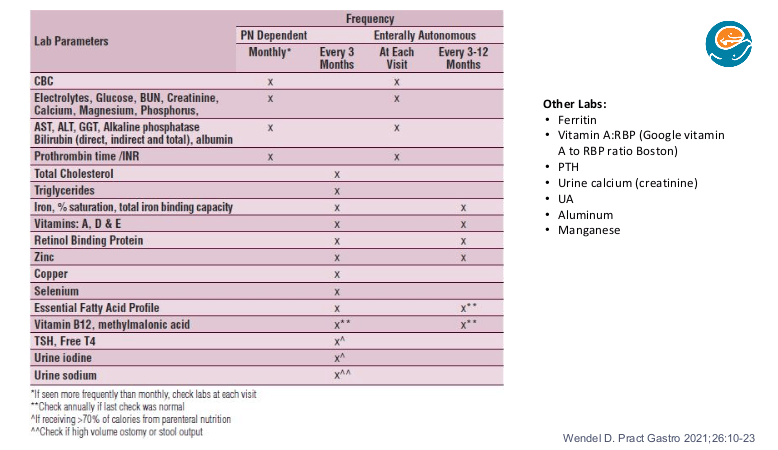
We had an brilliant lecture given to our group by Danielle Wendel who leads Seattle Children’s Intestinal Rehabilitation team. My notes below may contain errors in transcription and in omission. In addition, the information provided is based on what is done in Seattle. However, there is not a lot of evidence for much of what is done in intestinal rehabilitation. Thus, there is variation in practice at different centers and what works for one patient might not work for another. Following my notes, I have included many of her slides (same slides as yesterday’s post).
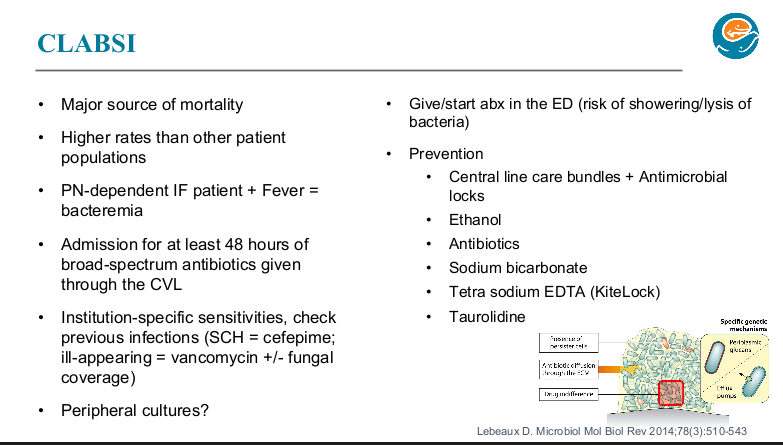
CLABSI Pointers:
- -At Seattle, with suspected CLABSI, usually central blood culture obtained without peripheral blood culture. (Peripheral blood cultures have not helped their team improve management)
- -Everyone with SBS and with fever (greater than or equal to 100.4) stays for at least 48 hrs on broad spectrum IV antibiotics (choice based on local sensitivities) through the central line until it is conclusively determined if they have a CLABSI (which still carry a significant mortality risk)
- -Sodium bicarbonate lock experience has been good (8.4% solution, 1.5 mL lock for the entire time off PN in all tunneled CVL flushed in at the end of the dwell). It has become a good substitute for ethanol locks. Their experience will be published soon. Since sodium bicarbonate lock does not need to be withdrawn, it has been associated with less line breakage. Several lock solutions (KiteLock and Taurolidine) are not currently available in the U.S. KiteLock is about to be studied in Seattle.
- -At Seattle, all CLABSI are treated through the line and every effort is made to salvage and/or repair lines. Line replacement increases risk of losing central IV access.
- -Line is removed for fungal infections
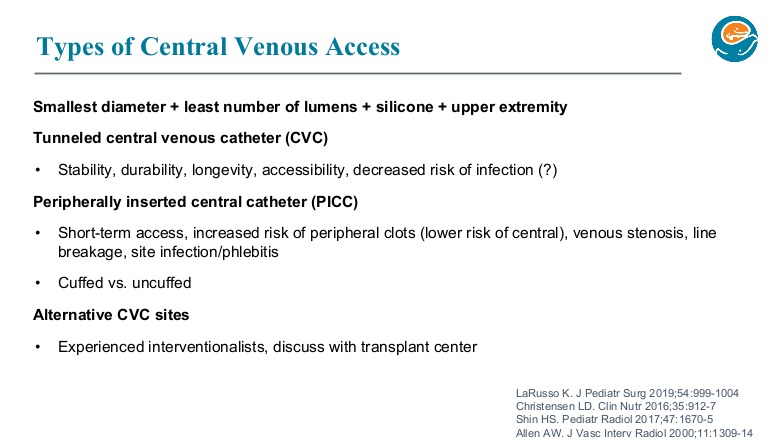
- -The Seattle team prefers tunneled CVC
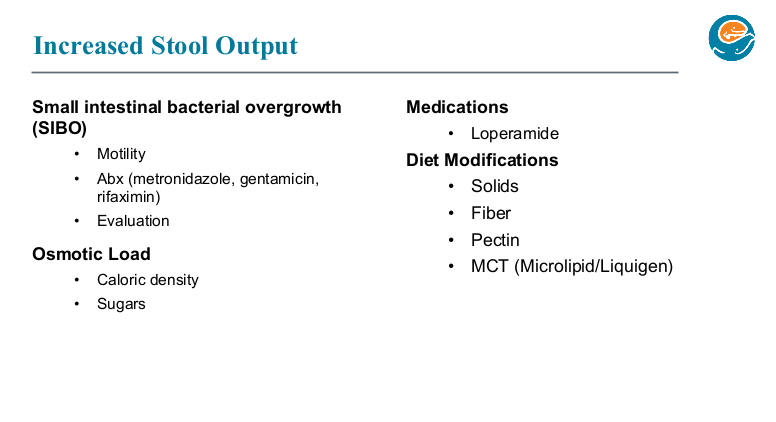
SIBO Pointers:
- -Testing is problematic. Breath tests are not reliable in kids with SBS. Duodenal aspirates are often not helpful and have a number of technical difficulties; also, it is unclear whether a duodenal aspirate is representative of the bacteria in the more distal bowel.
- -Metronidazole is their first line choice. Gentamicin (IV formulation given enterally) is their 2nd choice. Rifaximin is their 3rd line. Rifaximin would possibly be used earlier in treatment except for difficulty getting covered. When used, they crush up pills rather than have it compounded to avoid sweeteners.
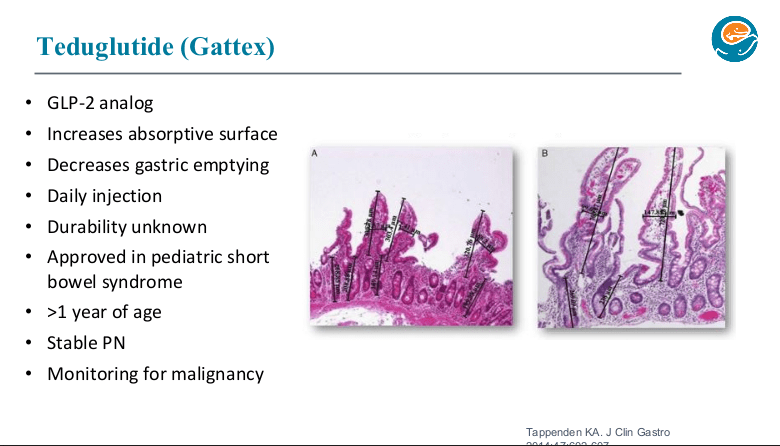
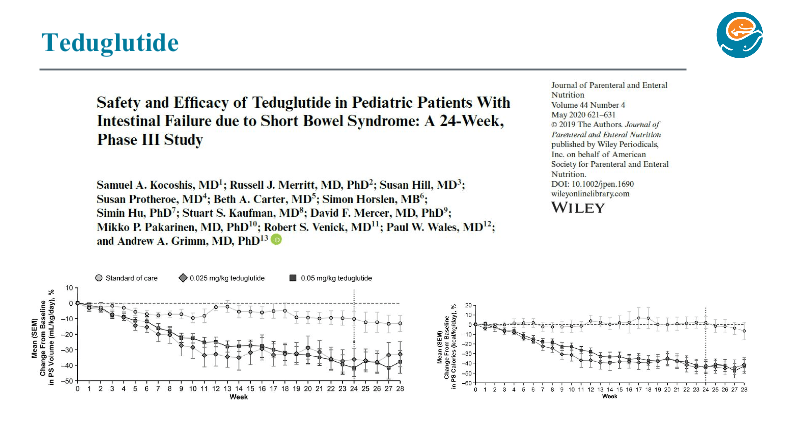
Teduglutide
- -Best to start if a patient is is > 1yo and on stable TPN (not able to wean)
- -Make sure patient is using a tiny needle (not adult needle in package)
- -Anticipate long-term treatment (?indefinite)
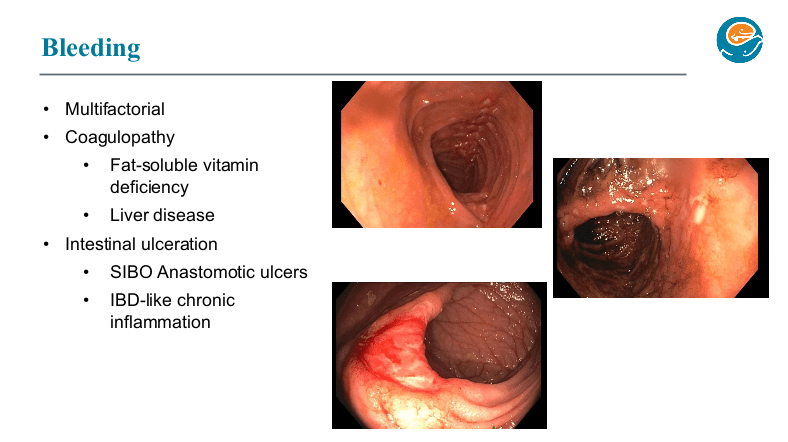
GI Bleeding Pointers:
- This is being seen frequently.
- Etiologies include anastomotic ulcers and IBD-like lesions. If a patient is not improving with standard approaches and possibly resection, could need an anti-TNF type agent.
- At Seattle, they are very selective about patients appropriate for a STEP procedure as this may be associated with more frequent bleeding over time due to the many staples used. Hand-sewn tapering may be a better option for many patients.
- With the challenging decisions required for these bleeding patients, discussion with an experienced intestinal rehab center may be helpful.

Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.