A recent study (PS Myles et al. NEJM 2018; 378: 2263-74, editorial 2335-6) throws some shade on the idea that restricting IV fluids during surgery results in better outcomes.
With ERAS (enhanced recovery after surgery) procedures, one of the components has been restricting IV fluids during surgery due to concerns that excessive fluid will result in bowel wall edema and slower recovery. To better determine if a restrictive IV fluid approach or a more liberal approach was better, this RELIEF study randomized approximately 3000 patients who were receiving major abdominal surgery into two arms: a restrictive group and a liberal group; they received a median of 3.7 liters of IV fluids and 6.1 liters respectively during and up to 24 hours after surgery.
Key findings:
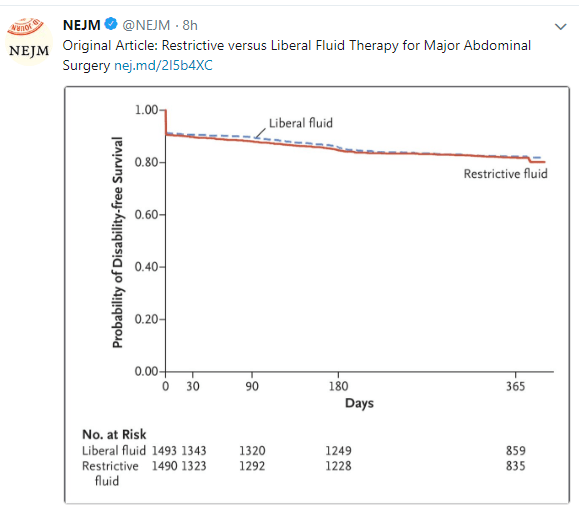
- Rate of disability-free survival at 1 year was 81.9% in the restrictive group and 82.3% in the liberal group (hazard ratio for death or disability was 1.05, CI 0.88-1.24, P=0.61)
- Rate of acute kidney injury was 8.6% in the restrictive fluid group compared to 5.0% in the liberal fluid group (P<0.001). Renal replacement therapy was 0.9% in the restrictive fluid group compared to 0.3% in the liberal fluid group (P=0.048).
- Rates of surgical site infection was 16.5% in the restrictive fluid group compared to 13.6% in the liberal fluid group (P=0.02). The authors speculate that this could be related to perfusion of surgical anastomosis.
The associated commentary notes that in this age of minimally invasive surgery, a modestly liberal administration of IV fluids does not create substantial fluid retention.
My take: Restrictive fluid regimen during major abdominal surgery resulted in higher rates of kidney injury and surgical site infections. This study indicates that for ‘enhanced recovery’ that a more liberal fluid regimen is safer.
Related posts:
- Fast Track Recovery/Enhanced Recovery After Surgery (ERAS is Awesome!)
- ERAS -Enhanced Recovery After Surgery (2016) With full slide set explaining ERAS further