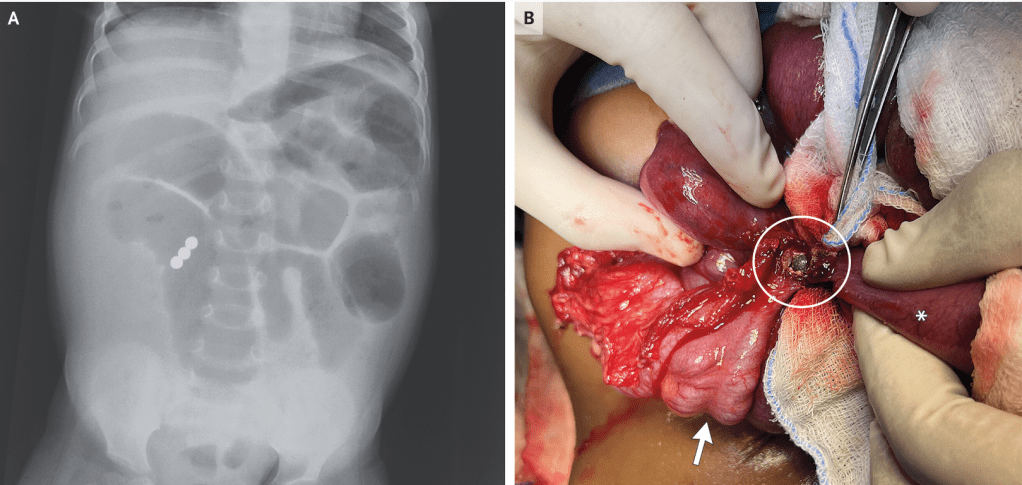
G Prasad, V Jain. N Engl J Med 2024;391: e48. Small-Bowel Obstruction and Intestinal Fistula from Accidental Ingestion of Magnets
Case presentation excerpt:
A previously healthy 18-month-old girl was brought to the emergency department with sudden-onset abdominal distention that had been preceded by 3 days of diarrhea and 1 day of vomiting…an emergency exploratory laparotomy was performed. An ileocecal fistula (Panel B, circle) created by the union of three magnetic beads was identified (arrow, cecum; asterisk, ileum), and dilated loops of bowel were noted. The bowel was repaired. The patient was discharged after five days.
My take: There are a lot kids admitted for multiple magnet ingestion. Even in well-appearing children, due to concerns for complications, they are often observed until progression of the magnets. However, it does seem that many do not advance well after working their way to the cecum.
Related blog posts:
- New Federal Safety Standard for Magnets to Prevent Deaths and Serious Injuries (2022)
- Capsule Motility –Better Than Corn? & Zen Magnets Recall Link (2021)
- Magnet Safety – screenshots from a recent (5/19/21) ‘tweetorial’ on Magnet Safety (other blog links on this post)
- Useful Endoscopic Tricks for Stricture Management and Magnets