Dr. Craig Friesen gave our group an excellent update on food allergy and disorders of brain-gut interaction (DGBIs). His main disclosure was that he is not an allergist. My notes below may contain errors in transcription and in omission. Along with my notes, I have included many of his slides.

Key points:
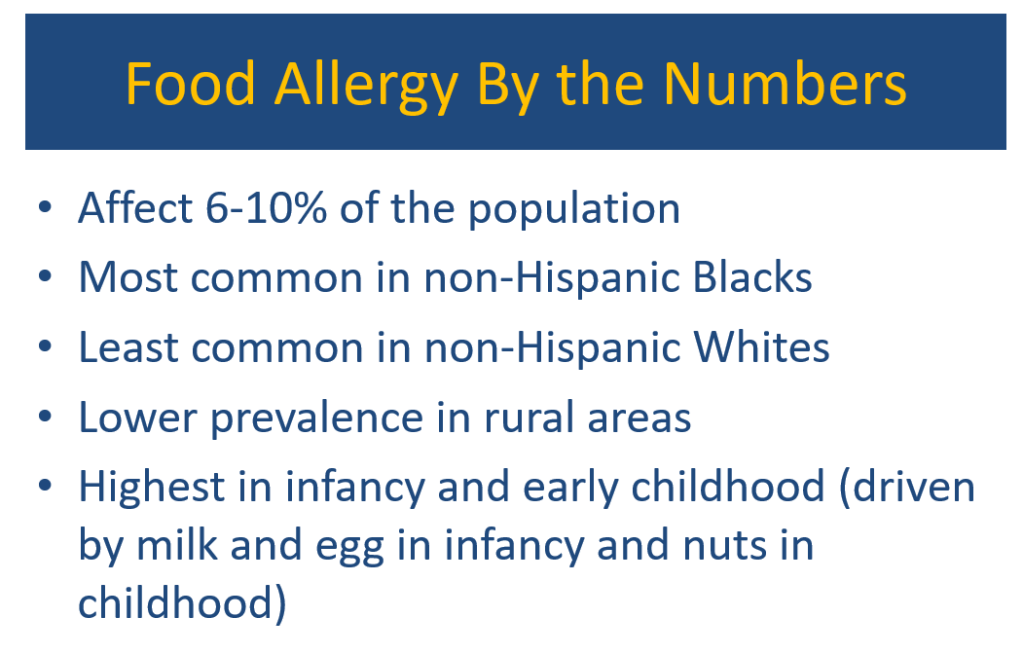
- Food allergies are common affecting 6-10% of the population. In infants, milk and egg are common allergens. Nut allergies are more frequently seen in children
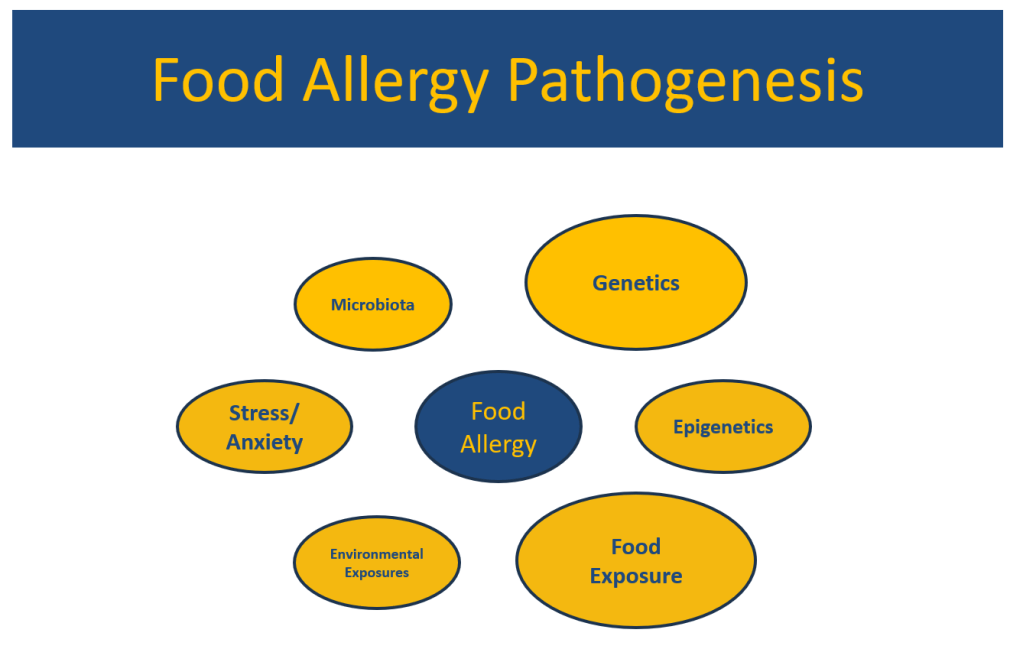
- There are likely hundreds of genes that can predispose towards allergies
- Food exposures, especially in the 4-6 month range, have been associated with a lower risk of food allergies
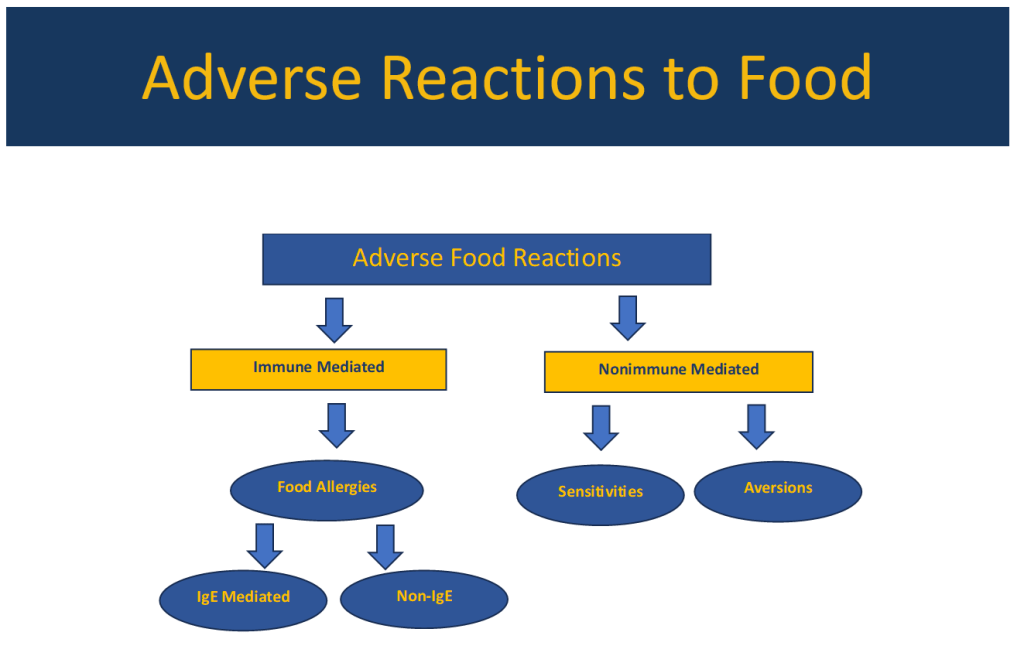
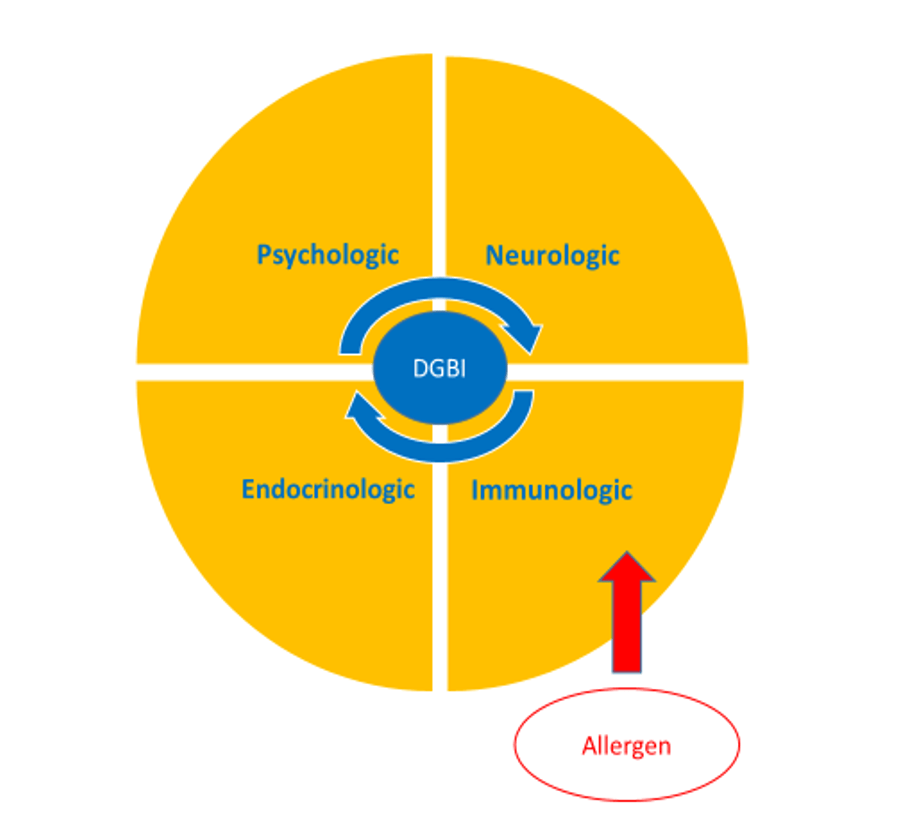
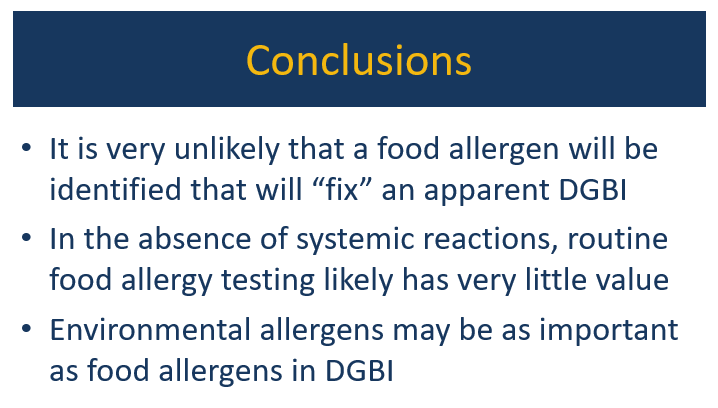
- Food trigger symptoms are present in most patients with DGBIs; however, the lines between immune mechanisms and non-immune mechanisms are often blurry
- Food allergy testing (skin prick testing, IgE-based blood tests) is not recommended in the absence of systemic symptoms due to poor specificity (perhaps ~10%). Obtaining a careful history is a very important part of determining allergies. Double-blind challenges, which are rarely done, are still considered “gold standard” for diagnosis
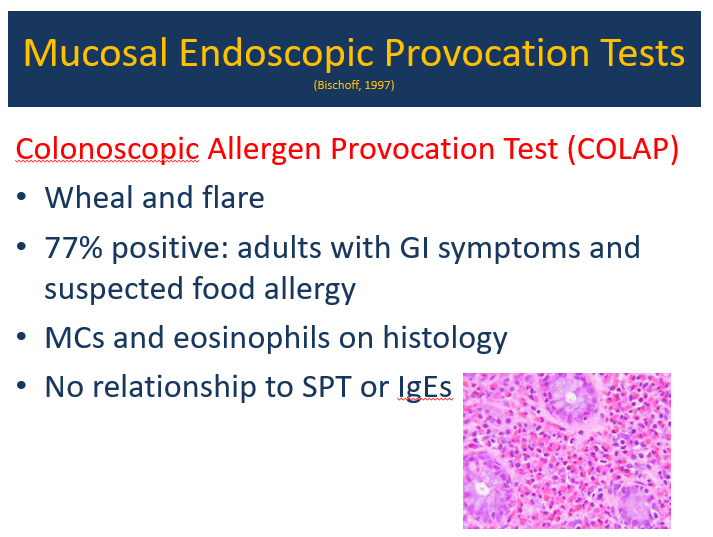
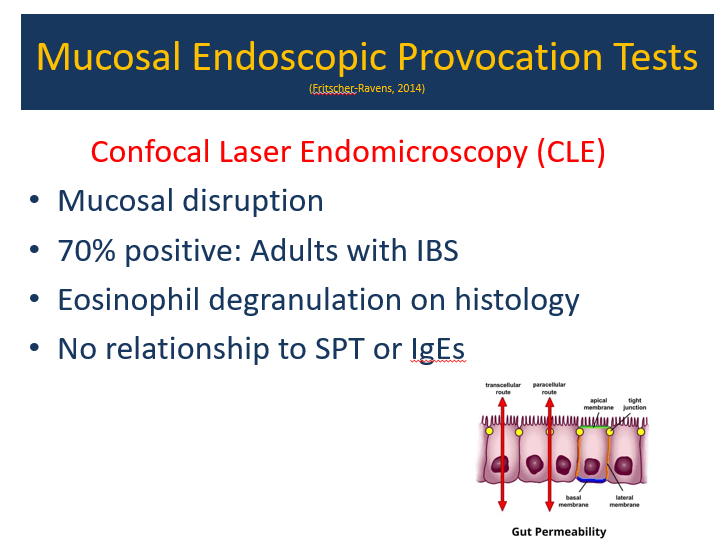
- Mucosal endoscopic provocation (research tool) often discloses localized immune reaction; it does not correlate with skin prick testing or IgE-based blood tests
- After prior sensitization/food allergies, stressful conditions may create similar symptoms as allergic exposures. This can be mediated by histamine and tryptase/mast cells
- It is rare for food allergen restriction to “fix” a DGBI. Occasionally, food allergies may be part of the problem. Dietary restrictions may lead to weight loss and contribute to ARFID
- IgG-based allergy testing (widely available) is not recommended; IgG antibodies are usually indicative of tolerance
- Environmental pollen counts are associated with increased DGBI symptoms, increased mucosal eosinophils, and less sleep
- Environmental allergen testing can sometimes be helpful in identifying cross-reacting foods
- Alpha-gal syndrome. Consider testing in those with symptoms triggered by meat ingestion, and those with refractory symptoms. In pediatric patients, often no rash is identified and many will ‘outgrow’ allergy
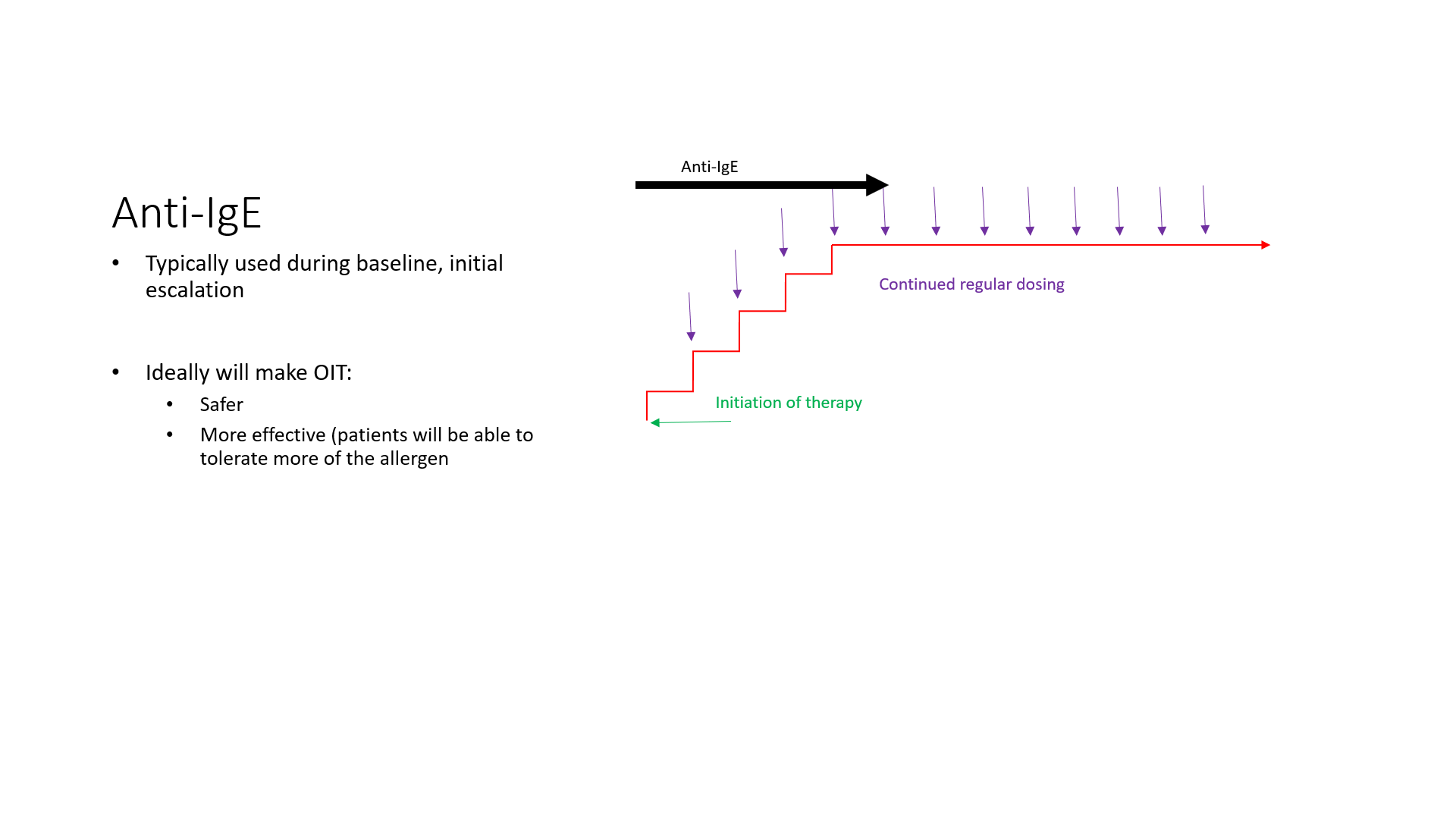
- Oral immunotherapy can be effective in improving tolerance for allergic foods; however, up to 70% will redevelop intolerance
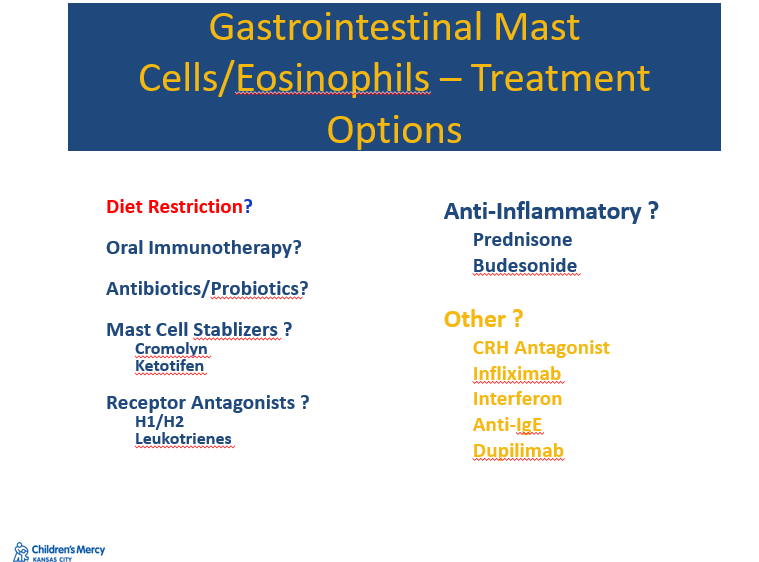
- When mucosal eosinophilia is identified, there are a number of potential treatments including dietary restrictions, mast cell stabilizers, antihistamines, and steroids








Related blog posts:
- “An Allergic Basis for Abdominal Pain”
- Is There a Way to Prove Which Dietary Factors Trigger IBS? RE: A Fritscher-Ravens et al. Gastroenterol 2019; 157: 109-18 –confocal laser endomicroscopy (CLE) for “real-time detection and quantification of changes in intestinal tissues” related to food challenges
- Dr. Victoria Martin: Management of Cow’s Milk Protein Allergy/Intolerance : Are We Causing More Harm Than Good? (Part 1)
- Dr. Victoria Martin: Management of Cow’s Milk Protein Allergy/Intolerance : Are We Causing More Harm Than Good? (Part 2)
- OUtMATCHing Food Allergies?
- “Separating Fact from Fiction in the Diagnosis and Management of Food Allergy”
- Quality Forum: Understanding Food Allergy Testing (Part 1)
- Quality Forum: Understanding Food Allergy Testing (Part 2) & Atopic Dermatitis
- Overdiagnosis of Milk Allergy in Infancy and New Consensus Recommendations
- Understanding Alpha-Gal Syndrome: Key Symptoms and Findings
- Nonanaphylactic Alpha-Gal and Chronic Gastrointestinal Symptoms (2023 Pediatric Study)
- Best Allergy Articles 2021 (Part 5): Allergy Test Ordering
- Eczema Rarely Linked to Food Allergy
- Allergy Prevention Strategy: Early Exposure Beneficial (Long-term Data for Peanuts)
- The Peanut Story -Skin Patch Chapter
- Poorly-Conceived Allergy Testing Can Lead to Unnecessary Diet Restrictions and Complications
- “The Truth About Allergies and Food Sensitivity Tests”
- What’s Wrong with “I Want My Kid Tested For Food Allergies” | gutsandgrowth
- How Allergy Testing Can Lead to More Allergies
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.