P Bose et al. JPGN 2022; 75: 514-520. Endoscopy in Infants With Gastrointestinal Bleeding Has Limited Diagnostic or Therapeutic Benefit
I read this article shortly after convincing a surgical colleague to explore a well-appearing 6 month old with gastrointestinal bleeding for a Meckel’s diverticulum rather than undergo endoscopy.
In this retrospective cohort study of hospitalized infants (n=56, =/< 12 months) with gastrointestinal bleeding, the authors reviewed endoscopic procedures (EGD, Colonoscopy, Flexible Sigmoidoscopy) with respect to identifying diagnosis and in terms of outcomes.
Key points:
- Seven endoscopies identified sources of GIB: gastric ulcers, a duodenal ulcer, gastric angiodysplasia, esophageal varices, and an anastomotic ulcer.
- Intervention for bleeding control occurred in just 3 cases (5.4%); two of these had liver disease.
- Most (55%) had no abnormalities on endoscopy
- The authors detail two fatal cases in which GIB started in the first week of life. Both had complications occurring within 3 hours of endoscopy, one with a gastric perforation and one with necrotizing enterocolitis.
My take: Endoscopy in infants with GIB is rarely beneficial. Supportive care and surgical interventions should be considered, especially in those without underlying liver disease.
Related blog posts:
- Timing of Upper Endoscopy with GI Bleeding -Is It Safer to Wait a Bit? | gutsandgrowth
- ACG Guideline: Upper Gastrointestinal and Ulcer Bleeding | gutsandgrowth
- Amazing Case Report: Speedy Recognition of an Aortoesophageal Fistula | gutsandgrowth
- Cutting Edge for Endoscopic Control of Bleeding | gutsandgrowth
- GI Bleeding -Forrest Classification
- All Bleeding Stops (part 2)
- All bleeding stops | gutsandgrowth
- Superior Results for Over-The Scope Clip for Severe UGI Bleeding
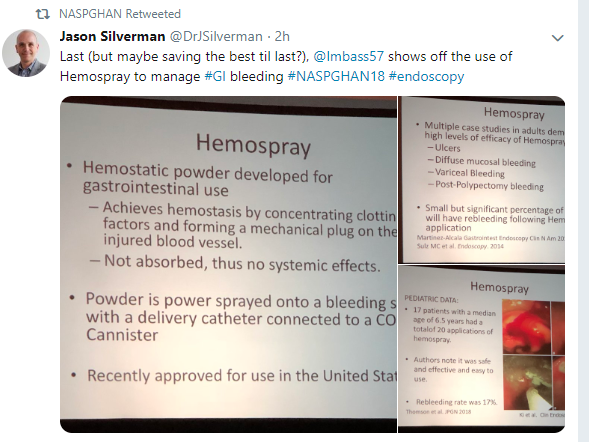
- Hemospray Efficacy and Rebleeding

Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.