MJ Temido et al. Am J Gastroenterol 2025;120:125–134. Drug-Induced Acne in Inflammatory Bowel Disease: A Practical Guide for the Gastroenterologist
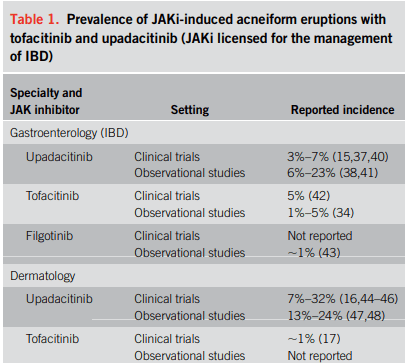
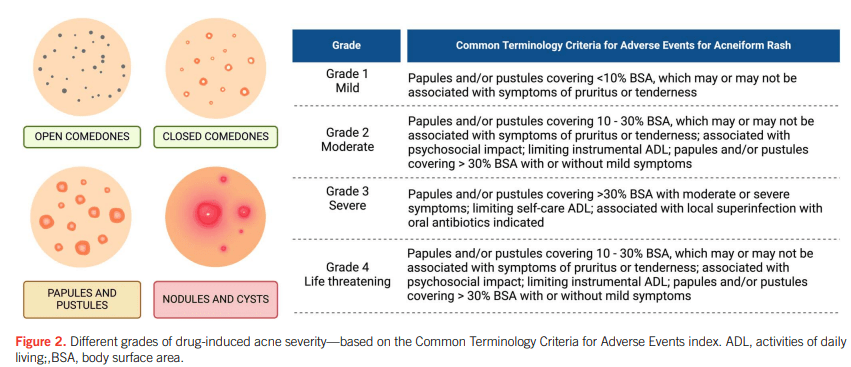
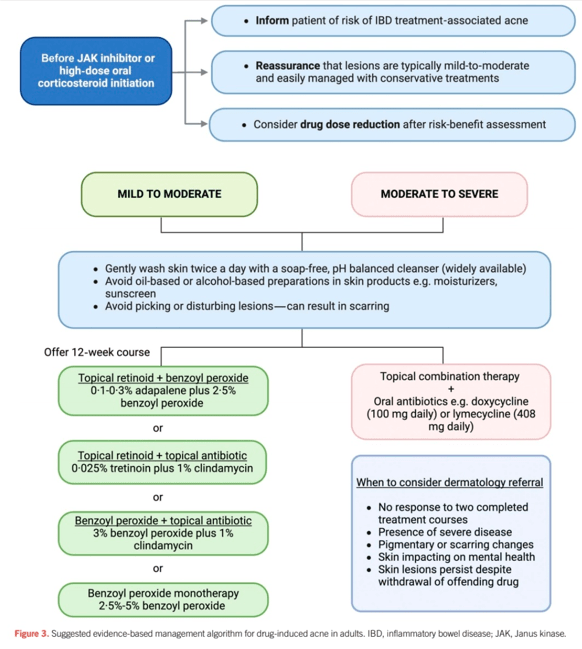
“Corticosteroids and Janus kinase inhibitors (JAKi) are commonly used for the treatment of inflammatory bowel disease (IBD) and are known to aggravate a prior tendency to acne or trigger the development of new acneiform eruptions. Both randomized controlled trials and real-world studies have identified acne as one of the most common treatment-emergent adverse events in JAKi… This review examines the characteristics of drug-induced acne in IBD treatments, provides a practical guide for gastroenterologists to manage mild-to-moderate occurrences, and highlights when to seek specialist dermatology advice.”
My take: This is a helpful review of acne management in the setting of IBD.
Related blog posts:
- More Data: Upadacitinib “is Effective and Safe” Plus 2 in Kids
- Landmark Study: Oral Biologic for Crohn’s –Upadacitinib
- New FDA Rinvoq (upadacitinib) Indication: Oral Treatment For Crohn’s
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.