6/17/25 Healio, E Bascom: Proposed Medicaid cuts could lead to thousands of preventable deaths annually
An excerpt:
Congress passing the controversial One Big Beautiful Bill Act could leave millions without insurance and lead to at least 16,000 annual preventable deaths, according to research published in Annals of Internal Medicine…
Arthur L. Caplan, PhD, a professor and founding head of the division of medical ethics at NYU Grossman School of Medicine, told Healio that the authors’ “warnings about what will happen should the Big Beautiful Bill go through have to be taken very seriously.”
“I think the fallout in terms of impact on Medicaid populations … people losing coverage who would then lose access [to health care] is morally staggering and unacceptable,” he said. “We are taking some of the most vulnerable people in society … and cutting back what is often somewhat meager benefits to begin with…”
A brief recently published by the Robert Wood Johnson Foundation also examined the potential impact of Medicaid cuts. Researchers revealed that, if the bill passes, national health care spending would drop by $797 billion over the next 10 years… They found that physicians would see an $81 billion cut, but hospitals would see the biggest decline in spending, at $321 billion.
Cited Study: A Gafney et al. Annals of Internal Medicine 2025; https://doi.org/10.7326/ANNALS-25-00716 Open Access! Projected Effects of Proposed Cuts in Federal Medicaid Expenditures on Medicaid Enrollment, Uninsurance, Health Care, and Health
An excerpt:
Enactment of the House bill advanced in May would increase the number of uninsured persons by 7.6 million and the number of deaths by 16 642 annually, according to a mid-range estimate…These estimates may be conservative. They rely on CBO’s assumption that states would replace half of the federal funding shortfall…Medicaid cuts would likely also increase uncompensated care, stressing hospitals and safety-net clinics and causing spillover effects on other patients…
ACA boosted enrollment to more than 90 million. Today, despite its many shortcomings, Medicaid enjoys wide support from the electorate and serves as the foundation of the nation’s health care safety net. The cuts under consideration, intended to offset the cost of tax cuts that would predominantly benefit wealthier Americans, would strip care from millions and likely lead to thousands of medically preventable deaths.
My take: Yogi Berra is attributed with the saying, “It’s tough to make predictions, especially about the future.” While this is true, it is highly likely that huge cuts in Medicaid funding will result in huge numbers who lose health insurance with subsequent increases in mortality and other adverse outcomes.
Related article: M Mineiro and M Sanger-Katz, NY Times 6/19/25: ‘Little Lobbyists’ Urge Senators to Oppose Trump’s Bill Cutting Medicaid

Related blog posts:
- How The IRS Proved That Health Insurance Saves Lives
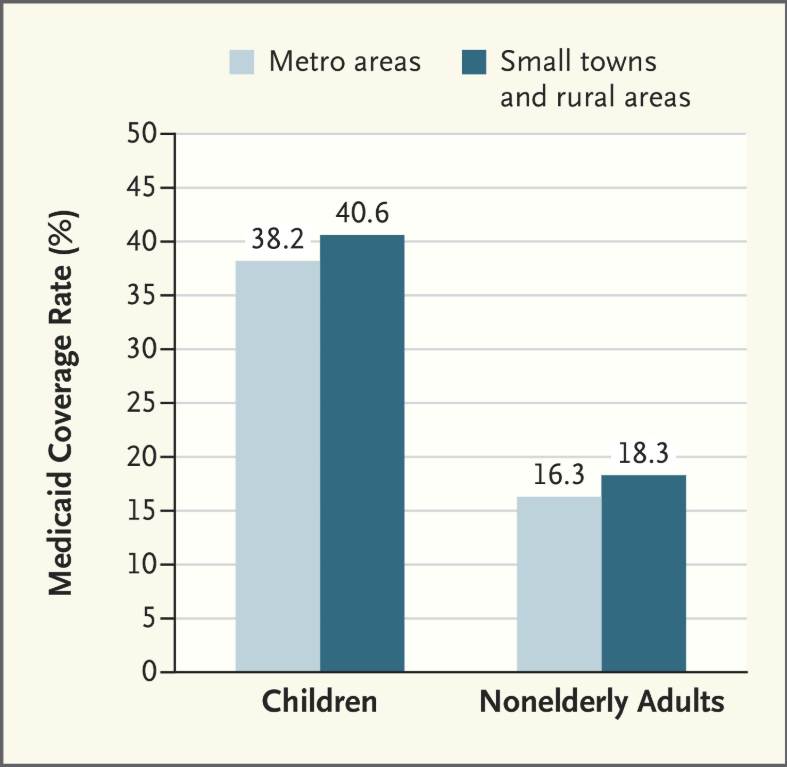
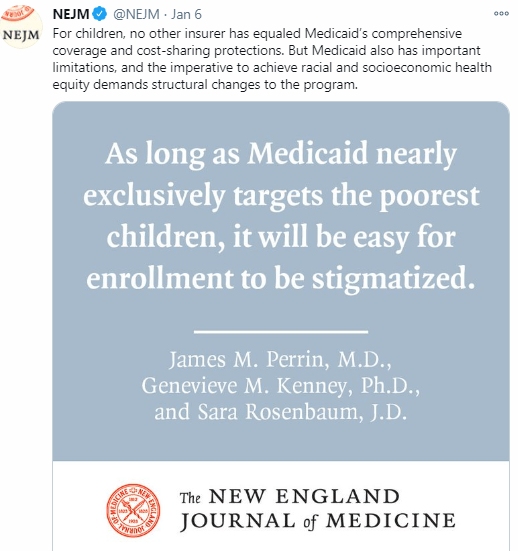
- Why the Proposed Medicaid Cuts Matter: Children and Other Vulnerable Populations Will Suffer
- High Rates of Denying Medical Care for Medicaid Patients Managed by Health Insurers
- How Putting America First is Undermining Health Outcomes Here and Globally
- Delays by Insurance Companies Result in Worse Outcomes for Children with Inflammatory Bowel Disease
- How to Successfully Appeal Health Insurance Denials
Personal Message: