Din, Shahida et al. The Lancet Gastroenterology & Hepatology; 2024: DOI: 10.1016/S2468-1253(24)00264-4. Open Access! Harms with placebo in trials of biological therapies and small molecules as induction therapy in inflammatory bowel disease: a systematic review and meta-analysis
Background: “Placebo-controlled trials are especially important during the early phases of drug development, as use of placebo aids early detection of efficacy or futility.”
Methods: The authors performed a systematic review which identified 47 trials including 20,987 patients (14 267 [68·0%] receiving active drug and 6720 [32·0%] receiving placebo) were eligible. The studies involved multiple RCTs of biologics and small molecules in IBD.
Key findings:
- The risks of worsening of IBD activity (Active treatment vs placebo: 563/13,473 [4·2%] vs 530/6252 [8·5%];RR 0·48)
- Withdrawal due to adverse event (Active treatment vs placebo: 401/13 363 [3·0%] vs 299/6267 [4·8%]; RR 0·62)
- Serious adverse event (Active treatment vs placebo: 682/14,267 [4·8%] vs 483/6720 [7·2%]; RR 0·69)
- Serious infection (Active treatment vs placebo: 140/14 ,194 [1·0%] vs 91/6647 [1·4%]; RR 0·67)
- Serious worsening of IBD activity (Active treatment vs placebo: 187/11,271 [1·7%] vs 189/5056 [3·7%]; RR 0·4)
- VTEs (Active treatment vs placebo: 13/7542 [0·2%] vs 12/2981 [0·4%]; RR 0·45)
- All of these adverse outcomes were significantly lower with active drug than placebo.
My take: Now that there are proven medications that are effective for moderate-to-severe Crohn’s disease, head-to-head trials of novel drugs against existing drugs with proven efficacy, rather than placebo-controlled trials, should be prioritized.
Related blog posts:
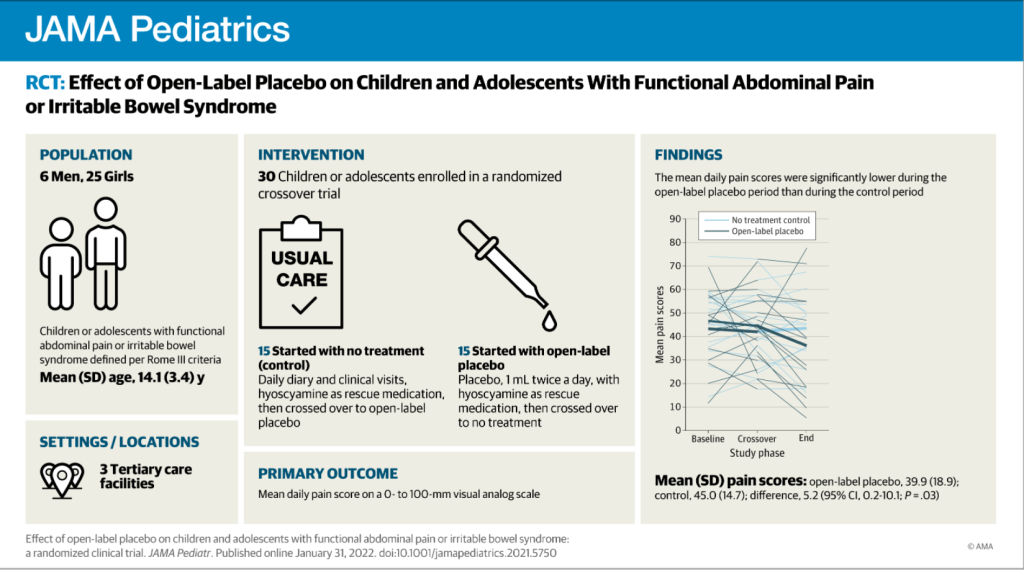
- How to Lower Placebo Effects in Crohn’s Disease Trials
- How to Get Rid of the Placebo Effect in IBD Trials (This blog link has some of my favorite advice at the bottom in the image)
- According to the study which you would never qualify for… (2023)
- According to the study which you would never qualify for…(2012)
- Comparative Evidence and Positioning Advance Therapies for Inflammatory Bowel Disease